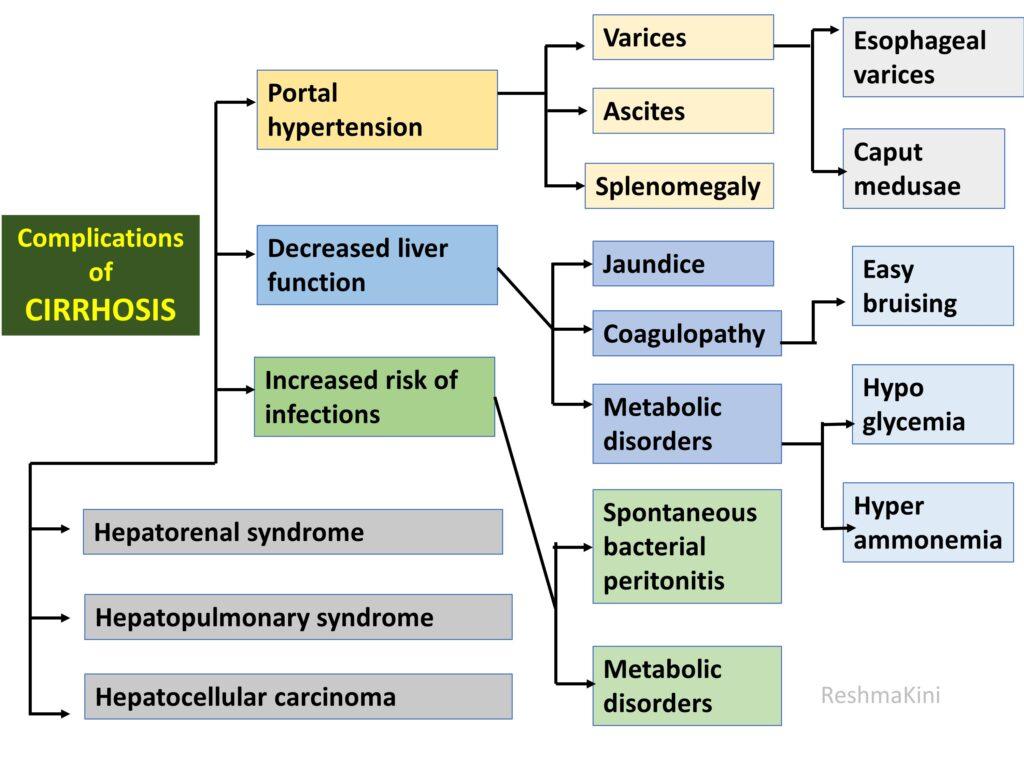
COMPLICATIONS OF CIRRHOSIS
Consequences of portal hypertension
1. Increased blood flow through porto caval anastomoses leads to development of dilated veins at the lower end of oesophagus. These protrude into the esophageal lumen and are prone to rupturing causing massive haemorrhage leading to death.
2. The dilated vessels around the umbilicus can give rise to medusa head appearance.
3. A combination of increased hydrostatic pressure in the splanchnic circulation and low oncotic pressure due to hypoalbuminemia will cause leakage of fluid into the peritoneal cavity producing ascites. This can develop infection.
4. Congestion of spleen can happen due to its connection to portal vein. The spleen enlarges. It can produce to pancytopenia
Consequences due to hepatocyte dysfunction
| Function Category | Specific Functions | Clinical Features of Cirrhosis Due to Functional Derangement |
|---|---|---|
| Metabolism | • Carbohydrate metabolism: glucose to glycogen storage, gluconeogenesis. | Hypoglycaemia (due to decreased glycogen storage and gluconeogenesis) |
| • Lipid metabolism: cholesterol synthesis, lipoprotein production, conversion of carbohydrates and proteins into fats | • Hyperlipidaemia | |
| • Protein metabolism: deamination of amino acid | • Muscle wasting and weakness (due to protein metabolism alterations) | |
| Synthetic function | Plasma protein synthesis (albumin, clotting factors), complement system components | Coagulation abnormalities, hypoalbuminemia and its consequences (oedema, ascites) |
| Detoxification | • Metabolising drugs and oestrogen | Gynaecomastia, adverse drug reactions |
| • Conversion of ammonia to urea. | • Hepatic encephalopathy (due to accumulation of ammonia and other toxins) | |
| Storage | • Storage of vitamins (A, D, E, K, B12) and minerals (iron and copper). | • Vitamin deficiency |
| • Glycogen, iron storage. | • Anaemia (due to iron storage disruption), disruption of glycogen metabolism | |
| Bile Production | • Production and secretion of bile, essential for digestion and absorption of fats and fat-soluble vitamins in the small intestine. | • Malabsorption and steatorrhea (due to decreased bile production affecting fat digestion) • Fat-soluble vitamin deficiencies |
| Blood Filtration | • Filtration of blood coming from the digestive tract | • Increased susceptibility to infections |
| Immune Function | • Part of the reticuloendothelial system (Kupffer cells): engagement in phagocytosis, capturing and digesting bacteria, fungi, parasites, worn-out blood cells, and cellular debris. | • Increased susceptibility to infections due to impaired immune function |
Consequences other than due to hepatocyte dysfunction
| Complication | Pathogenesis | Clinical Consequences |
|---|---|---|
| Portal Hypertension | Increased resistance to blood flow through the liver due to scarring and nodules. | Blood rerouted into portocaval anastomotic sites producing varices. • At oesophagus - Risk of rupture and life-threatening bleeding. • At umbilicus- caput medusa Increasing hydrostatic pressure in portal circulation along with hypoalbuminemia causes ascites Congestive splenomegaly- Anaemia, leukopenia, and thrombocytopenia with onset of hypersplenism. |
| Ascites | Caused by portal hypertension and hypoalbuminemia. | Abdominal discomfort, risk of bacterial peritonitis. |
| Spontaneous Bacterial Peritonitis (SBP) | Infection of the ascitic fluid without an apparent source. | Abdominal pain and fever. |
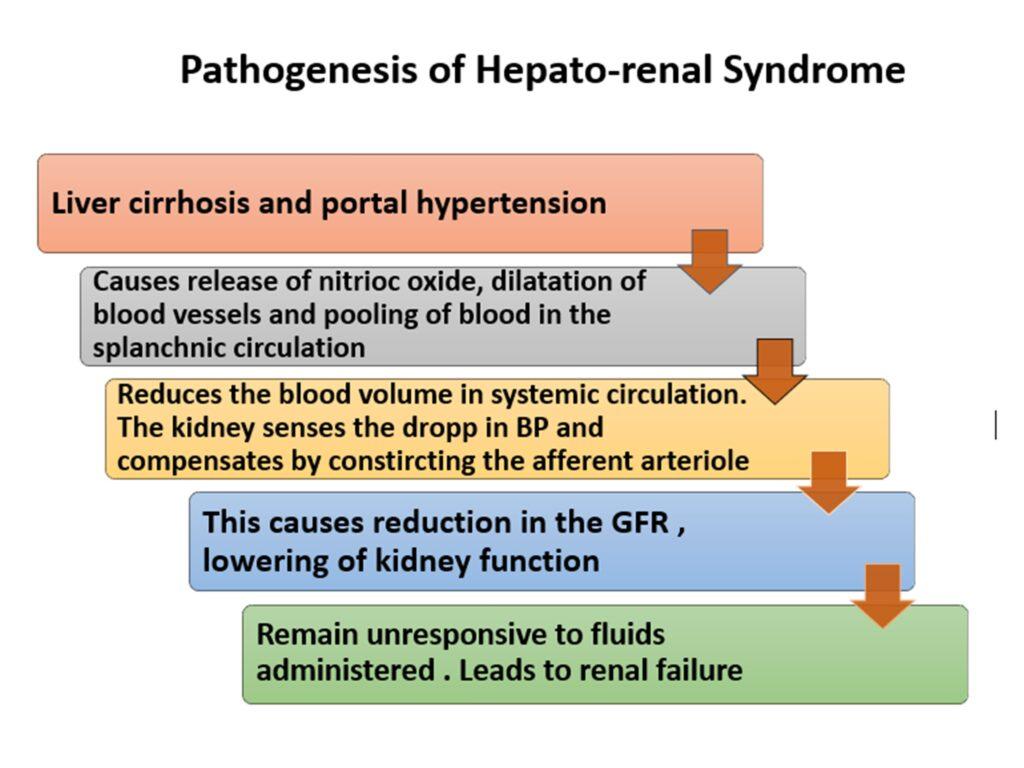
| Hepatorenal Syndrome | Kidney failure due to alterations in blood flow within the kidneys. | Significant kidney impairment and poor prognosis. |
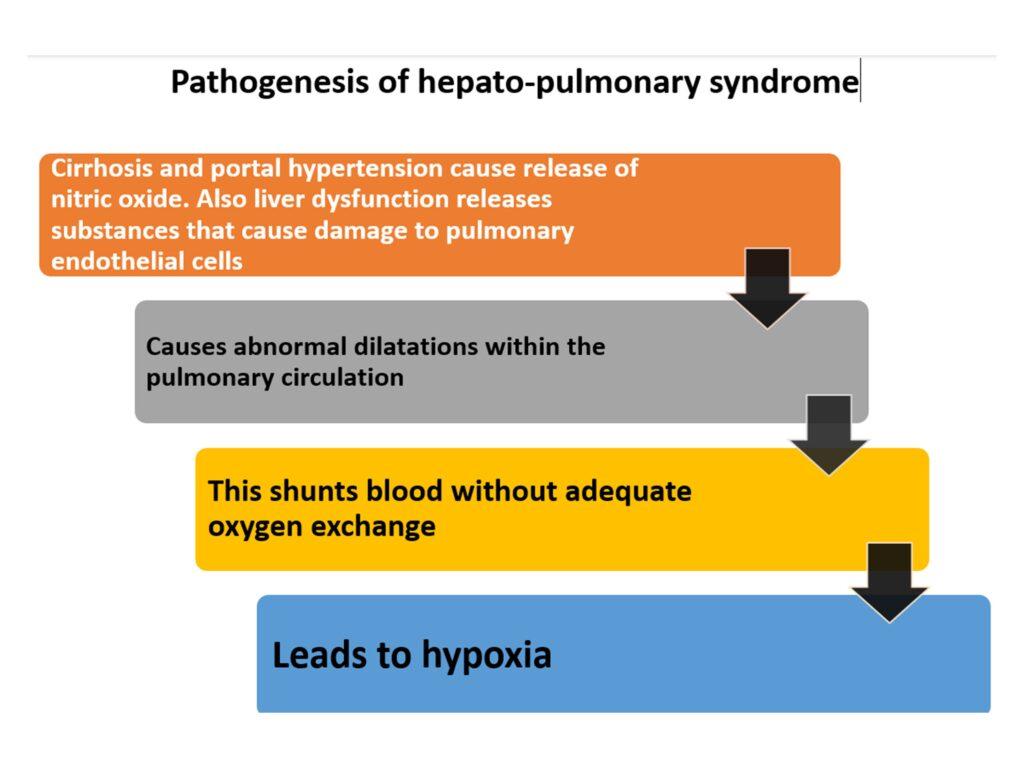
| Hepatopulmonary Syndrome | Formation of bypassing blood vessels in the lungs. | Difficulty breathing and decreased oxygen levels. |
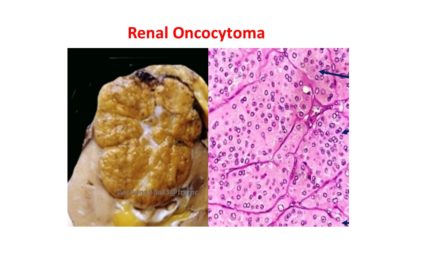
| Hepatocellular Carcinoma | Long-standing inflammation and liver cell turnover. | Leading cause of death in cirrhosis patients, impacts treatment and prognosis. |
Click here to read CIRRHOSIS PART 1



Recent Comments