Anatomy of the Liver:
Lobes: The liver is divided into four lobes: the right lobe, left lobe, caudate lobe, and quadrate lobe.
Segments: Each lobe is further subdivided into functional units called segments. There are eight segments in total, numbered I to VIII.
The liver is enveloped by a connective tissue capsule called Glisson’s capsule, which extends into the liver as fibrous septae. These septa divide the liver into small functional units called lobules.
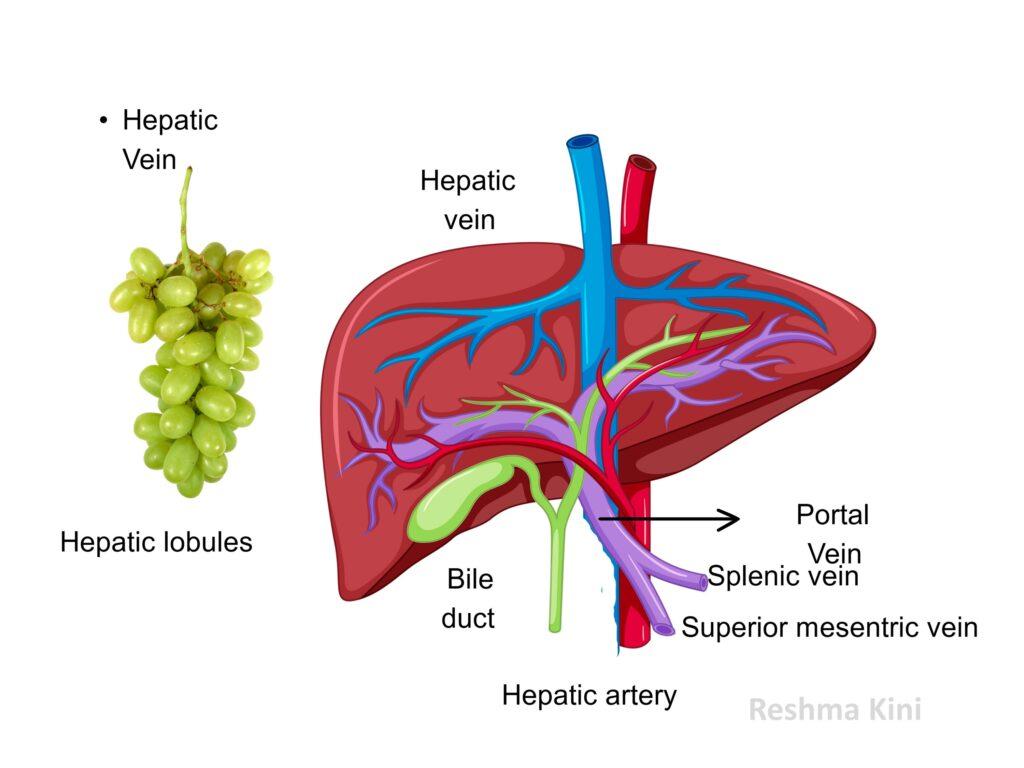
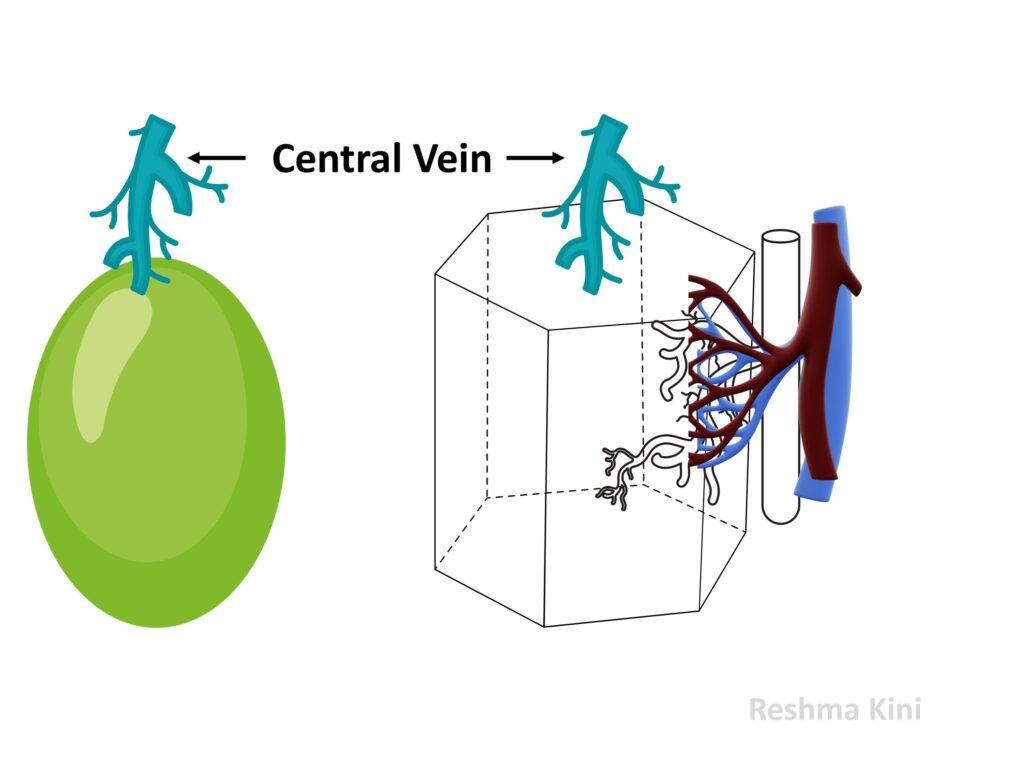
Hepatic lobule:
It is a structural unit of the liver. It is a three-dimensional hexagon with a central vein at its centre. The central veins of each lobule join ultimately to give rise to the hepatic vein which drains into the Inferior vena cava
Blood Supply:
The liver receives blood from two sources: the hepatic artery and the portal vein.
The hepatic artery delivers oxygenated blood to the liver, while the portal vein brings nutrient-rich, partially deoxygenated blood from the digestive organs. These blood vessels enter the liver at the porta hepatis and branch extensively throughout the organ and branches of them are found at the corners of each hexagon
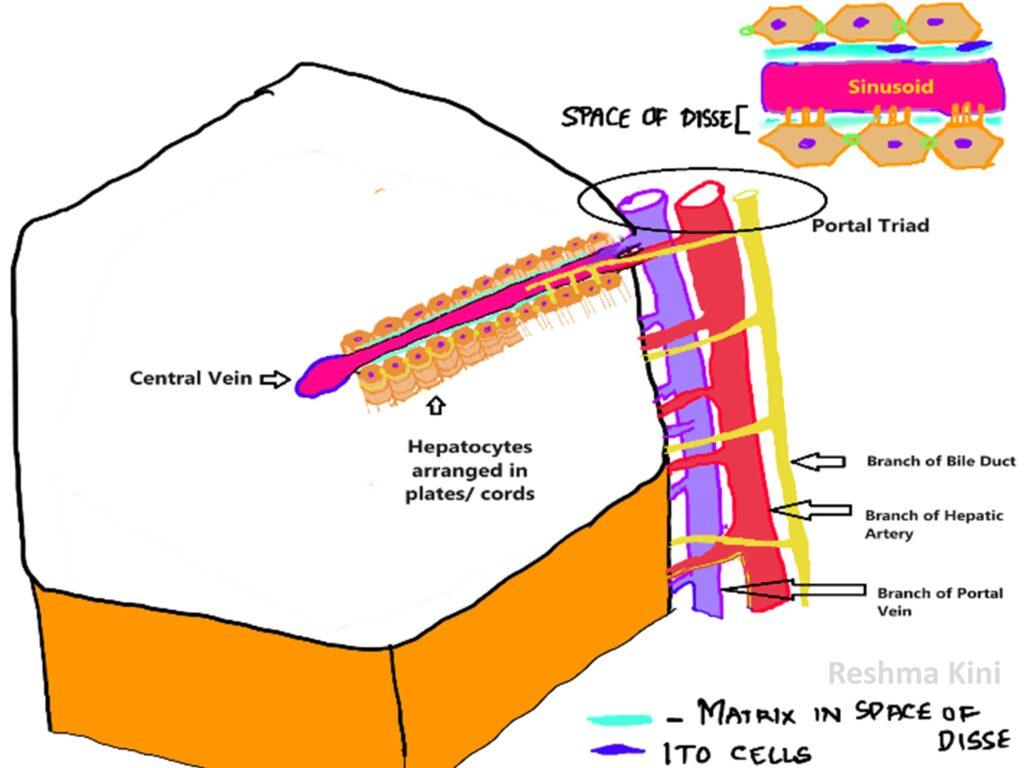
At the corners of the hexagon are the portal triads. Each portal triad has a branch of the portal vein, a branch of hepatic artery and a branch of the bile duct.
The blood pours into the hepatic lobule from the portal triad and travels towards the central vein within sinusoids.
These sinusoids are lined by endothelium and separated from the hepatocytes by a space containing Ito cells (Vitamin A storing cells) and some matrix. This is space of Disse.
Bile flows from hepatocytes into the bile canaliculi (ductules) and then continues its journey through the Canals of Hering towards larger bile ducts situated at the portal triad.
Portal vein
The portal vein is formed from joining of splenic and the superior mesenteric vein (SMV). The splenic vein drains the spleen, stomach, and the latter part of the colon. The SMV drains small intestine, parts of the large intestine, and associated structures.
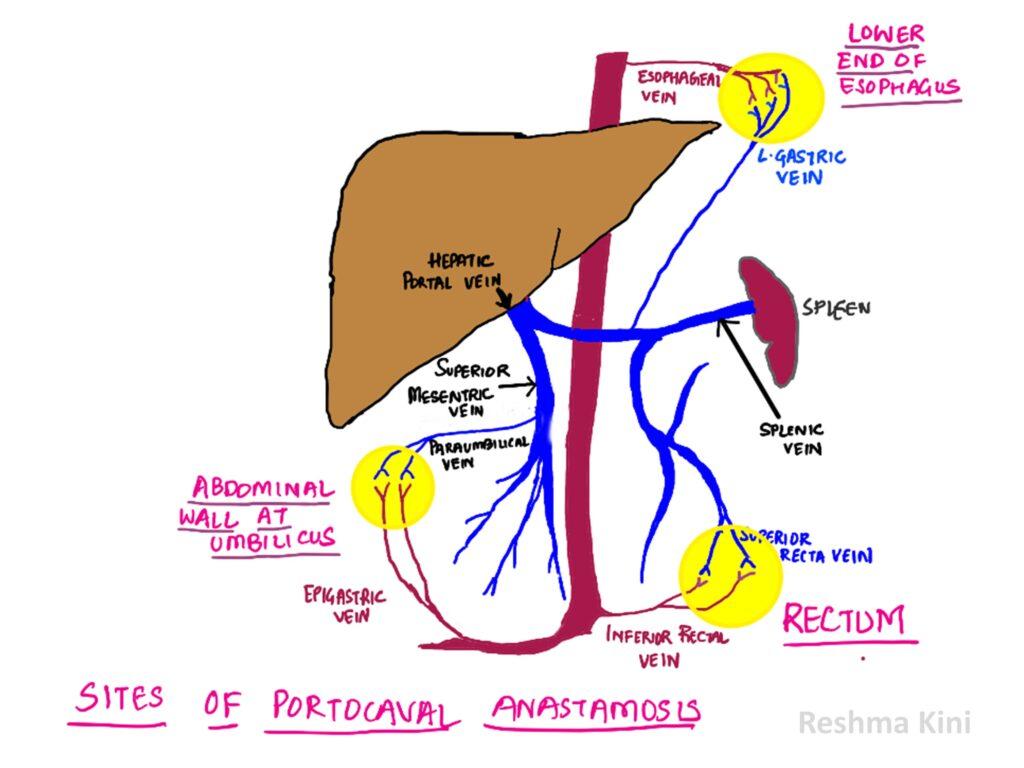
Porto-Caval Anastomoses
There are three significant areas where drainage occurs both by the tributaries of portal veins and those of the Inferior vena cava.
If the portal vein is unable to drain that area the connections between the two systems enable blood in portal system to bypass and directly enter the IVC. The vessels in these areas dilate and are called varicosities.
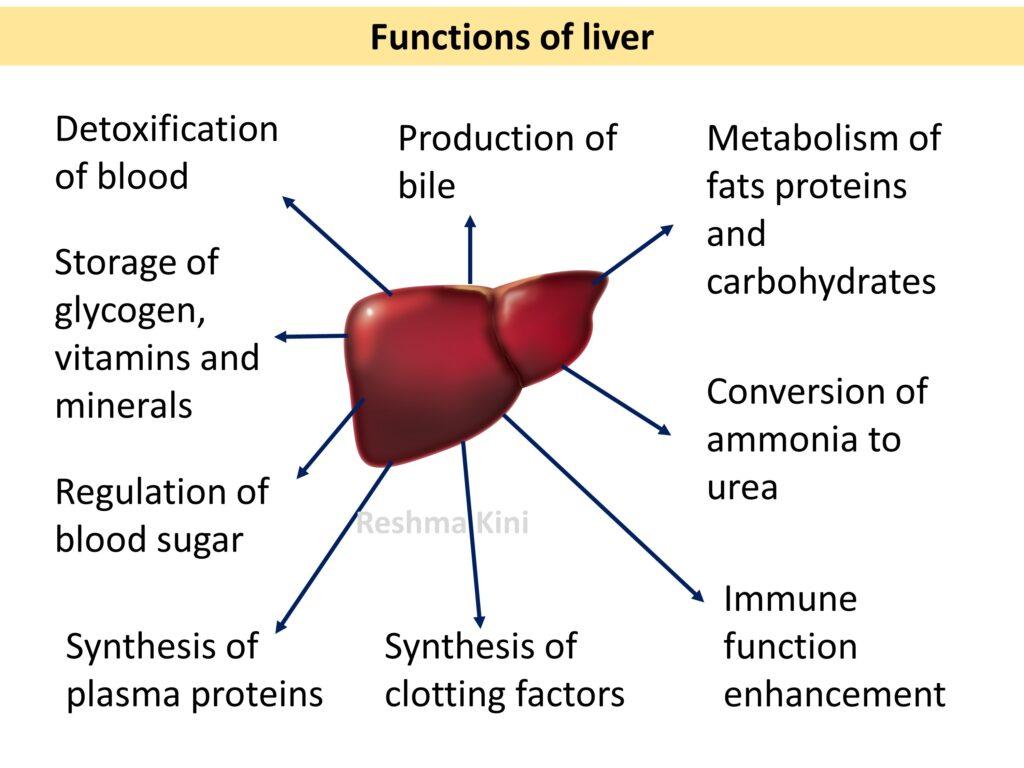
Functions of liver
CIRRHOSIS- PATHOGENESIS
Basic pathology concepts required to understand cirrhosis
I. Cell Injury and Inflammation – these explains the aetiology of cirrhosis
II. Healing- by regeneration and repair- this explains the pathogenesis
III. Physiologic functions of liver and Congestion and Oedema- explains the complications and clinical features
I. Inflammation-is the key initiator of cirrhosis.
Inflammation is a response to injury.
The entities that injure liver leading to chronic inflammation (Aetiology of cirrhosis) include-
• Chronic consumption of alcohol, (Chemical Injury)
• Chronic hepatitis B, Hepatitis D or hepatitis B+D, (Microbiological Injury)
• Non-alcoholic fatty liver disease (NAFLD) or non-alcoholic steatohepatitis (NASH) (Chemical Injury)
• Autoimmune hepatitis (Immunological Injury)
• Chronic bile duct obstruction or disease (such as primary biliary cholangitis or primary sclerosing cholangitis) (Chemical Injury)
• Hemochromatosis (excessive iron accumulation in the liver) (Chemical and free radical Injury)
• Wilson’s disease – copper accumulation in the liver (Chemical Injury)
• Alpha-1 antitrypsin deficiency (Injury due to protein misfolding)
• Chronic exposure to toxins or medications (Chemical Injury)
• Cystic fibrosis (Multiple causes)
• Glycogen storage diseases (Chemical Injury)
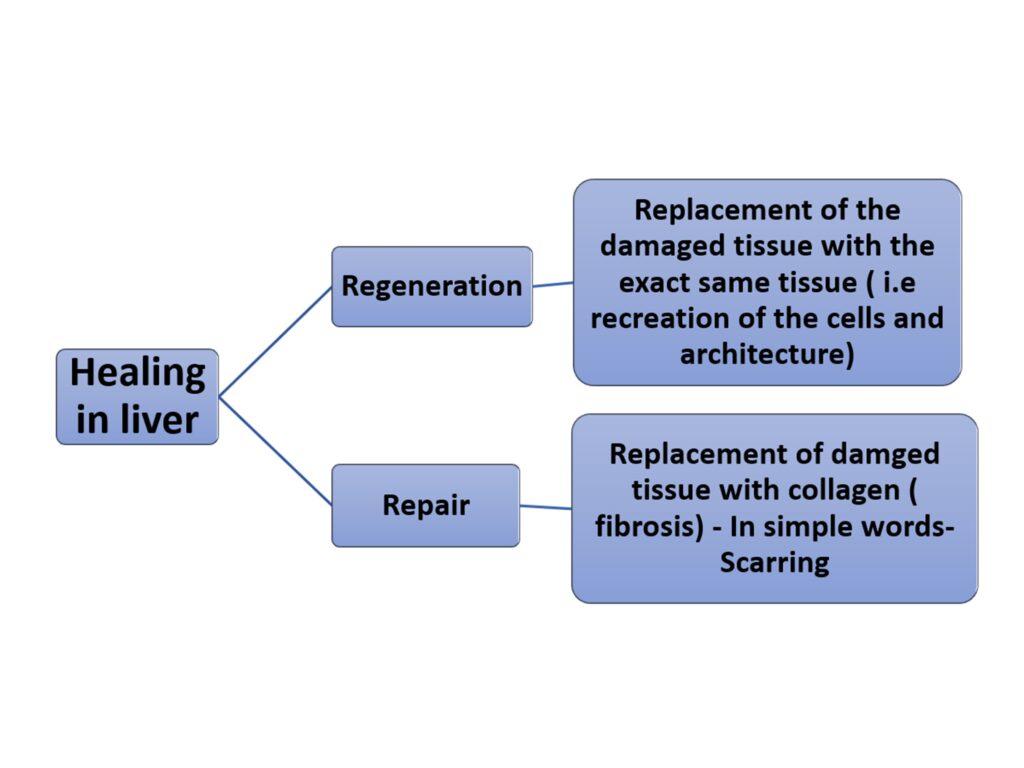
II. Healing
Following inflammation there is healing. Unlike in most other organs the liver tends to heal by two mechanisms- regeneration and repair
Following inflammation initially the liver tends to regenerate. With time however it shifts healing towards the repair and starts laying down collagen (fibrosis).
Fibrosis first begins in Space of Disse and is initiated by Ito cells. These cells under the influence of inflammatory mediators transform into hepatic stellate cells which lay down collagen. The collagen is laid down between the central vein and portal triads and eventually between the portal triads themselves.
Result
1. The collagen in the space of Disse forms a physical barrier between the hepatocytes and the sinusoids and closes off exchange between the two.
This prevents:
• nutrients from reaching the hepatocytes -causing hepatic synthetic and metabolic function derangement and hepatocyte death and dysfunction
• hepatocytes from releasing important materials into sinusoids- like albumin and coagulation factors- leading to their deficiency
• hepatocytes picking substances from blood that are normally metabolised by them – ammonia, drugs, oestrogen and inhibiting their metabolism and leading to accumulation of such substances in the body producing the clinical features.
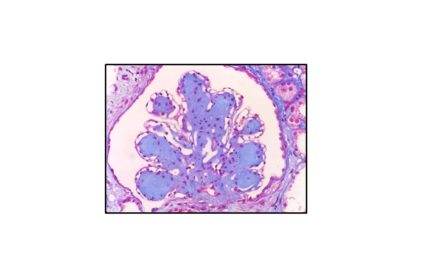
2. The process of damage, and fibrosis continues. The surviving hepatocytes attempt regeneration.
The result is extensive bands of scar tissue (collagen) within the liver interspersed by the regenerative nodules created by the surviving hepatocytes.
Due to presence of extensive fibrosis, the surviving hepatocytes are unable to recreate the original architecture.
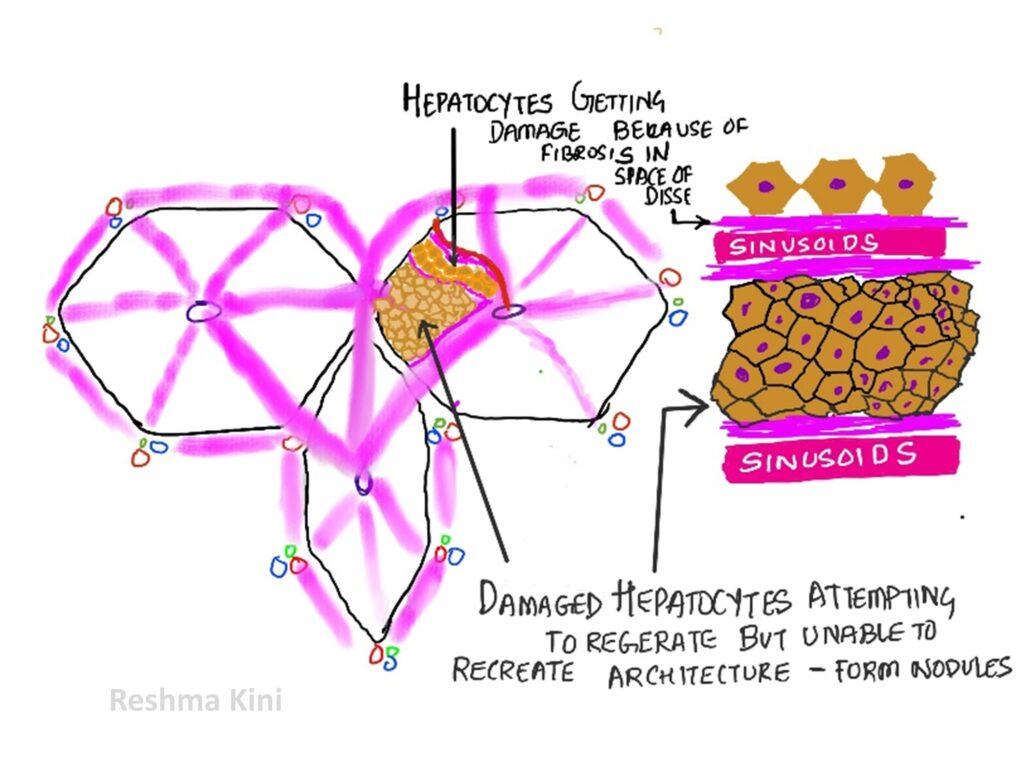
The entire liver loses its lobular architecture and becomes composed of small nodules either small( micronodular) or big ( macronodular >3mm in diameter)
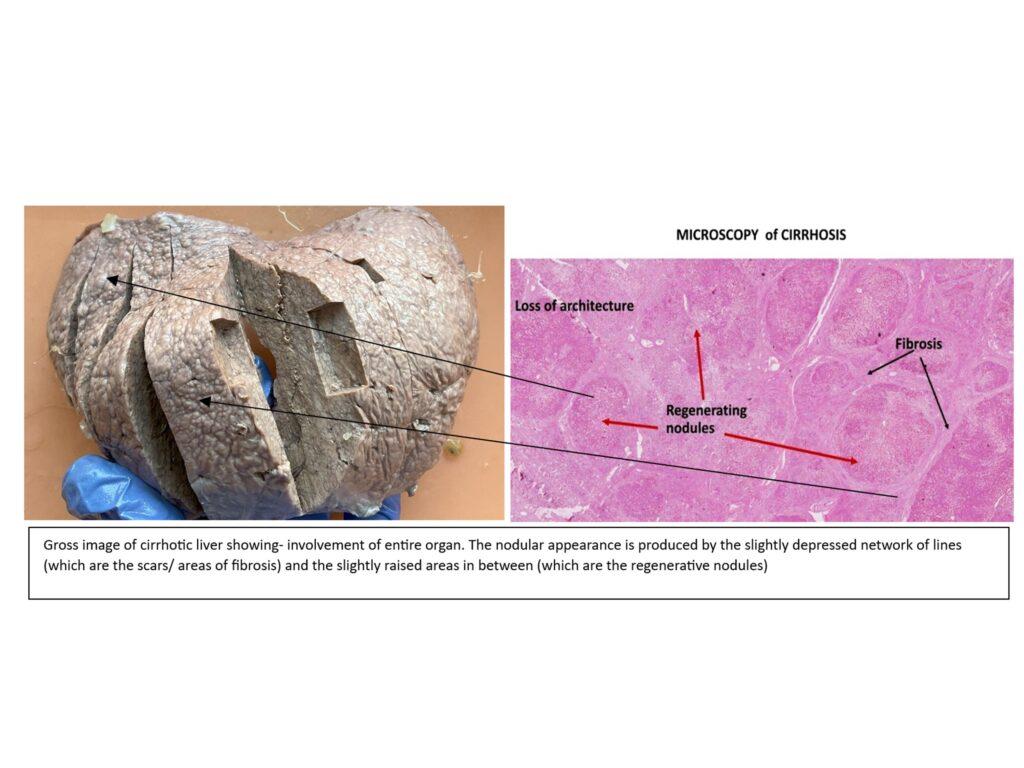
3. The regenerative nodules do not have the correct arrangement of the portal triad and the central vein. This results in hampering of proper blood flow and bile flow through the liver.
4. The resistance to blood flow in the distorted vessels put a backward pressure on the portal vein. The portal vein dilates (Portal Hypertension).
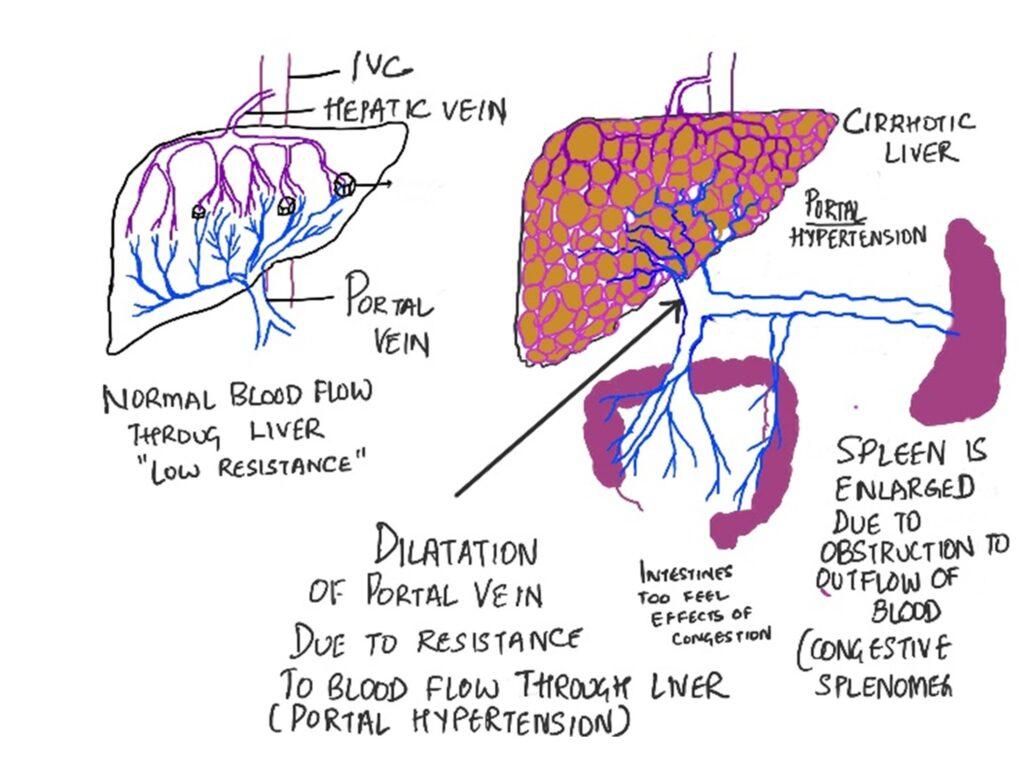
5. The pressure experienced by the portal vein is transmitted to its tributaries leading to congestion of spleen (Congestive splenomegaly) and intestines (dysfunction)
Consequences of cirrhosis are due to:
1. Hepatocyte dysfunction
i. Deficiency of albumin and coagulation factors in blood
ii. Increase in levels of ammonia in blood leading do encephalopathy( brain dysfunctions)
iii. Accumulation of metabolites in blood which are normally processed by liver- estrogen,, drugs
iv. Derangement of glucose, protein and lipid metabolism
2. Portal hypertension
a. Opening of the porto-caval shunts
i. Oesophageal varices
ii. Caput medusae
b. Congestive splenomegaly
3. Ascites
4. Hepatorenal syndrome- renal failure
5. Hepato-pulmonary syndrome. – breathing difficulty
6. Hepatocellular carcinoma
Continue to read CIRRHOSIS Part 2
Click here to watch the Video




Recent Comments