Celiac Disease: Understanding the Basics
Celiac disease, also known as Celiac sprue or Gluten-Sensitive enteropathy, is a chronic immune-mediated disorder that occurs in genetically predisposed individuals. It is triggered by the ingestion of gluten-containing foods such as wheat, rye, and barley.
Causes and Risk Factors
Celiac disease occurs in individuals who carry the HLA DQ2 and HLA DQ8 genes. Environmental factors, such as infections, low birth weight, and antibiotic use, are also proposed risk factors.
Pathophysiology
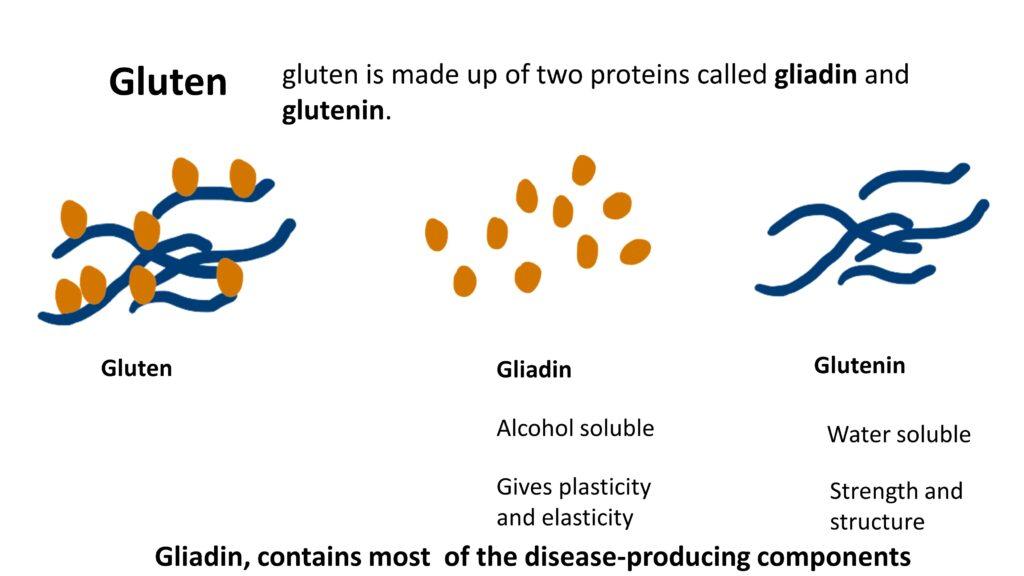
Gluten, a storage protein found in grains, is the major culprit in celiac disease. It consists of two proteins: gliadin and glutenin. Gliadin, the alcohol-soluble component, contains most of the disease-producing components.
When the intestinal epithelial cells are stressed, they express the MICA antigen. Consumption of gluten stimulates the production of interleukin-15 (IL-15) by epithelial cells, leading to the proliferation of intraepithelial lymphocytes. These activated lymphocytes express the NKG2D receptor, which interacts with MICA, resulting in damage to the epithelial cells.
In the lamina propria, deamidated gliadin interacts with antigen-presenting cells, stimulating CD4-positive T lymphocytes. This activation leads to the production of interferon gamma and other chemicals that further damage the epithelial cells.
Clinical Presentation
Celiac disease presents with various clinical features. Gastrointestinal symptoms include diarrhea, abdominal pain, bloating, and weight loss. Children may experience failure to thrive and growth retardation.
Nutritional deficiencies due to malabsorption can result in deficiencies of iron, vitamin D, vitamin B12, folic acid, and zinc. Skin manifestations can include itchy blistering skin lesions or dermatitis herpetiformis. Non-gastrointestinal symptoms, such as neurological symptoms, can also occur.
Diagnosis
Diagnosing celiac disease involves non-invasive and invasive methods. Non-invasive tests include detecting antibodies such as IgA antibodies against tissue transglutaminase, IgA antibodies against anti-endomysium, and IgA or IgG antibodies against gliadin peptides. However, these tests alone are not sufficient to confirm the diagnosis.
If non-invasive tests are positive, an endoscopy and duodenal biopsy are performed. The characteristic histopathological findings, in the presence of antibodies, confirm the diagnosis of celiac disease.
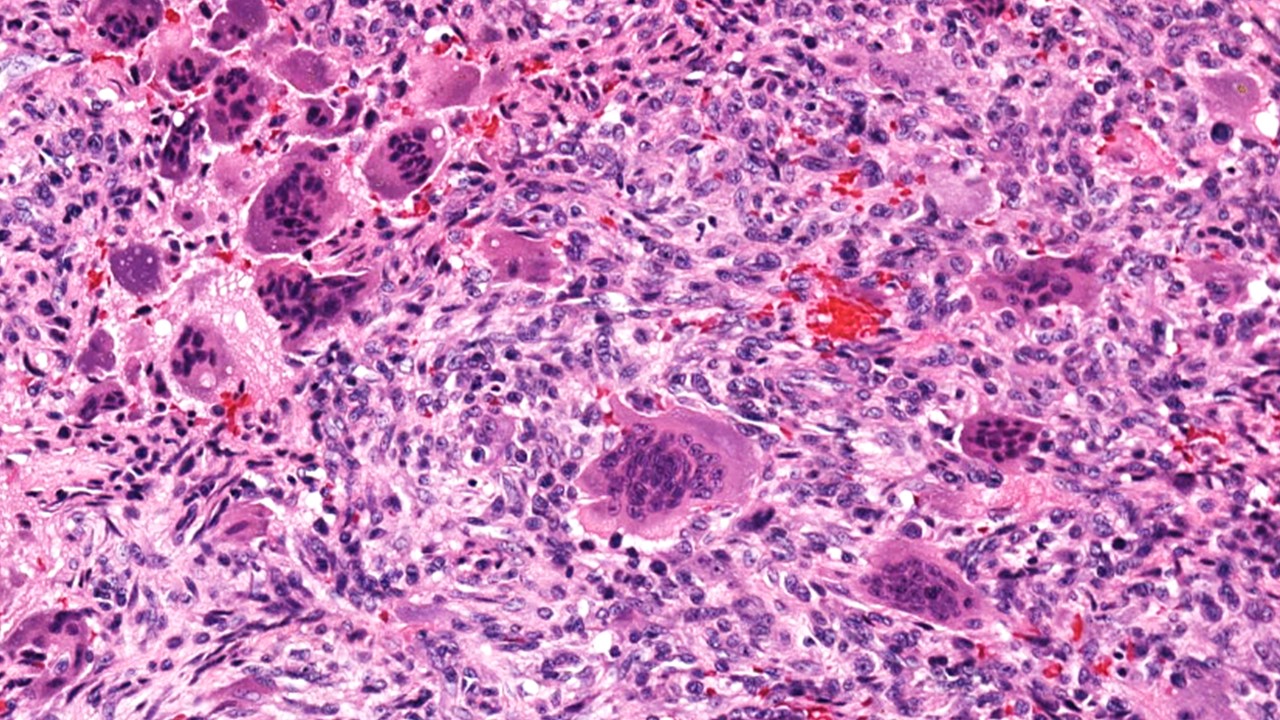
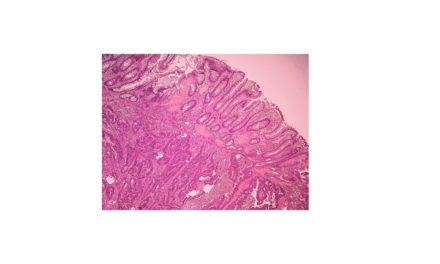
Histopathological Features
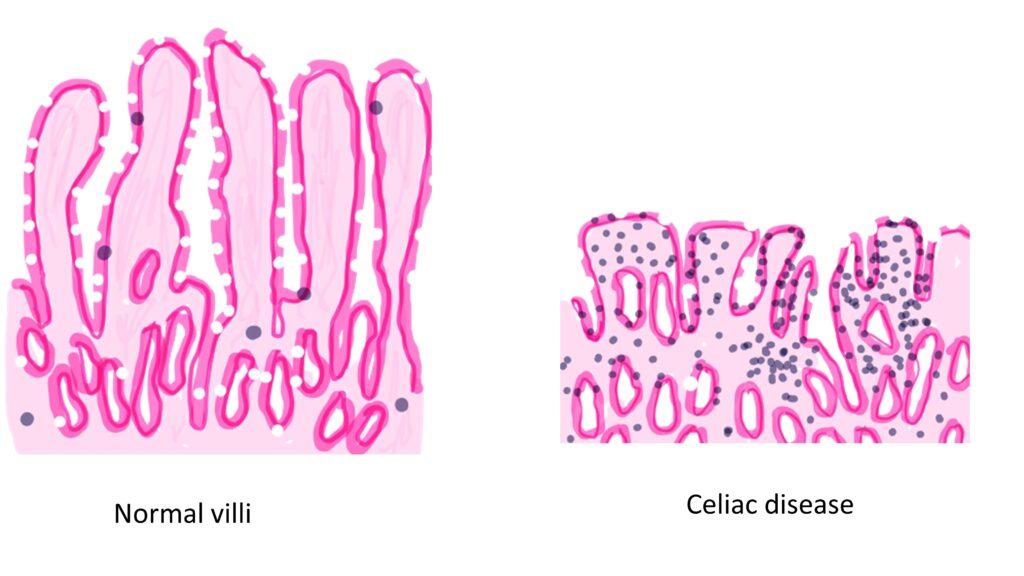
The histopathological features of celiac disease involve the small intestine. Microscopic examination of duodenal biopsies reveals characteristic findings:
Increased numbers of intraepithelial lymphocytes: There is an increase in the number of lymphocytes within the epithelial layer of the small intestine ( >20lymphocytes/100 epithelial cells).
Disruption of normal villous architecture: The finger-like projections called villi, which normally increase the surface area for nutrient absorption, become blunted or flattened.
Crypt hypoplasia: The small intestinal crypts, responsible for cell renewal, may appear reduced in number or size.
Villous shortening: The villi become shorter than normal, further compromising nutrient absorption.
Treatment
The only current treatment for celiac disease is a strict gluten-free diet. Adhering to this diet can lead to the resolution of symptoms, reduced antibody titers, restoration of normal or near-normal mucosal histology, and a reduction in the risk of long-term complications.
Complications and Associated Malignancies
In some cases, symptoms persist despite adherence to a gluten-free diet, indicating refractory sprue or a possibility of cancer in patients with celiac disease.
The major malignancies associated with celiac disease include:
Enteropathy-associated T-cell lymphoma: This is an aggressive lymphoma of intraepithelial lymphocytes that can arise in the small intestine.
Small intestinal adenocarcinoma: This is another important type of malignancy seen in celiac disease, characterized by the development of cancerous cells in the small intestine.
Regular follow-up and monitoring of individuals with celiac disease are crucial to detect any potential complications or malignancies at an early stage.
CLICK HERE to watch the tutorial on Celiac disease



Recent Comments