SQUAMOUS PAPILLOMA
Squamous papilloma is a benign growth that occurs on the surface of the skin or mucous membranes. It is characterized by finger-like projections or papillae, which are made up of an overgrowth of squamous epithelial cells.
Squamous papillomas can occur at various sites in the body, but some of the most common locations include:
Skin: Squamous papillomas can develop on the skin, particularly in areas that are frequently exposed to sunlight, such as the face, neck, arms, and hands.
Oral cavity: Squamous papillomas can occur in the mouth, including on the tongue, tonsils, and inside the cheeks.
Larynx: Squamous papillomas can develop on the vocal cords and other areas of the larynx, causing symptoms such as hoarseness and difficulty breathing.
Genital area: Squamous papillomas can develop on the genitals, including on the penis, vulva, vagina, and anus. These are often caused by HPV infection.
Nasal cavity and sinuses: Squamous papillomas can occur in the nasal cavity and sinuses, causing symptoms such as nasal congestion and difficulty breathing.
Esophagus: Squamous papillomas can develop in the esophagus, causing difficulty swallowing and other symptoms.
Etiology:
Squamous papillomas can be caused by a variety of factors, including infection with the human papillomavirus (HPV), smoking, or exposure to other irritants.
However, in the vast majority of cases, HPV is the underlying cause of squamous papillomas. There are over 100 different strains of HPV, and some strains are more likely to cause squamous papillomas than others. HPV types 6 and 11 are the most common causes of squamous papillomas in the oral cavity and respiratory tract
Pathogenesis:
HPV infects the cells of the skin or mucous membranes and can cause them to divide and grow abnormally, leading to the formation of a papilloma.
The exact mechanism by which HPV causes squamous papilloma is not completely understood, but it is thought to involve the E6 and E7 viral oncoproteins produced by the virus. These proteins can interfere with the normal regulation of cell growth and division, leading to the formation of abnormal growths.
When HPV infects cells, it can integrate its genetic material into the host cell’s DNA, leading to the expression of viral oncoproteins. These oncoproteins can interfere with the normal functioning of cellular proteins that regulate cell growth and differentiation. As a result, cells infected with HPV can begin to divide and grow uncontrollably, forming a squamous papilloma.
The development of squamous papilloma is also influenced by other factors, such as the immune system’s response to the virus, genetic factors, and environmental factors such as exposure to certain chemicals or toxins. These factors can affect the ability of the body to control HPV infection and may contribute to the formation of squamous papilloma.
Clinical features:
They are typically asymptomatic, but may cause pain or tenderness if located in areas of friction or pressure. Squamous papillomas may occasionally bleed and may cause cosmetic concerns. If located in the mouth or throat, they may cause difficulty swallowing, hoarseness, or a change in voice.
Diagnosis:
A healthcare provider can diagnose squamous papilloma through a physical examination. Additional tests such as a biopsy may be performed to confirm the diagnosis. I
Macroscopic findings:
can vary depending on the location and size of the growth, but it is typically characterized by finger-like projections or papillae that extend from the surface of the skin or mucous membrane. These projections can be smooth or irregular and may range in color from flesh-colored to pink or red.
Squamous papillomas are typically small and can be as small as a few millimeters or as large as several centimeters in diameter. They are usually round or oval in shape and have a raised, firm texture.
If the squamous papilloma is located in the mouth or throat, it may appear as a white or grayish-white growth with a rough or bumpy surface. In the genital area, squamous papillomas may appear as small, soft, wart-like growths or raised, flat lesions.
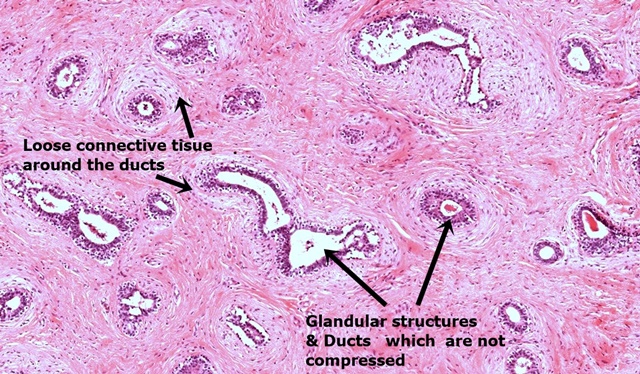
Microscopic features:
squamous papillomas are characterized by finger-like projections, called papillae, that are covered by layers of squamous cells. The papillae contain blood vessels and connective tissue – PAPILLOMATOSIS
The surface of the papillae is covered by a layer of stratified squamous epithelium, which may show mild to moderate HYPERKERATOSIS (thickening of the outer layer of skin) and ACANTHOSIS (thickening of the epidermis).
In cases of HPV-induced squamous papilloma, the infected cells may show characteristic changes, including koilocytosis (abnormal cell shape and size with a “halo” appearance), increased nuclear-to-cytoplasmic ratio, and hyperchromasia (increased staining intensity of the nucleus).

KOILOCYTES:
Koilocytes are abnormal squamous epithelial cells that are commonly associated with human papillomavirus (HPV) infections. These cells are characterized by a distinct morphology on microscopic examination, which includes the following features:
Enlarged, irregular nucleus: The nucleus of a koilocyte is typically larger than a normal squamous epithelial cell and has an irregular shape. The chromatin (DNA and protein) within the nucleus may appear clumped or granular. Often has a characteristic RAISIN ( irregular nuclear membrane – wrinkled appearance) like nucleus.
Perinuclear cytoplasmic clearing: The cytoplasm of a koilocyte appears to be pushed to the outer edge of the cell, creating a clear halo or “halo zone” around the nucleus. This is caused by the accumulation of viral proteins and other cellular debris in the perinuclear region.
Abundant eosinophilic cytoplasm: The cytoplasm of a koilocyte is usually abundant, granular, and stained pink with eosin, a common stain used in histology.
Koilocytes are not specific to squamous papilloma, but are also seen in other HPV-related lesions, such as genital warts and cervical dysplasia. Their presence on microscopic examination is a helpful clue to the diagnosis of HPV infection. However, the absence of koilocytes does not rule out the possibility of HPV infection or squamous papilloma, particularly if the lesion is small or has undergone extensive degeneration.


Recent Comments