LABORATORY DIAGNOSIS OF CANCER
What are the laboratory methods used to diagnose cancer?
There are several laboratory methods used to diagnose cancer, including cytopathological examination, histopathological examination, flow cytometry, molecular techniques (such as PCR, FISH, and NGS), and liquid biopsy. These methods play a crucial role in accurately diagnosing cancer and providing important insights into tumor characteristics and management.
What is cytopathological examination and how does it contribute to cancer diagnosis?
Cytopathological examination involves the study of cells to diagnose cancer. It can be done through two main methods:
exfoliative cytology and interventional cytology.
Exfoliative cytology involves the spontaneous shedding of cells from the lining of an organ into the underlying body cavity. A common example is the Pap smear used to detect cervical lesions. On the other hand,
Interventional cytology involves the active collection of cells through procedures like fine needle aspiration. This method allows pathologists to obtain cellular material from suspected malignant lumps or masses. Cytopathological examination helps identify abnormal cells and determine if they are cancerous, aiding in the diagnosis and subsequent management of cancer.
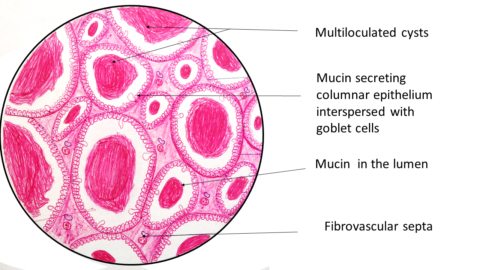
How does histopathological examination contribute to cancer diagnosis?
Histopathological examination plays a crucial role in cancer diagnosis by analyzing the microscopic features of tumors. Tissue samples can be obtained through various methods such as
Needle biopsy,
Endoscopic biopsy,
Incision biopsy, or
Excision biopsy.
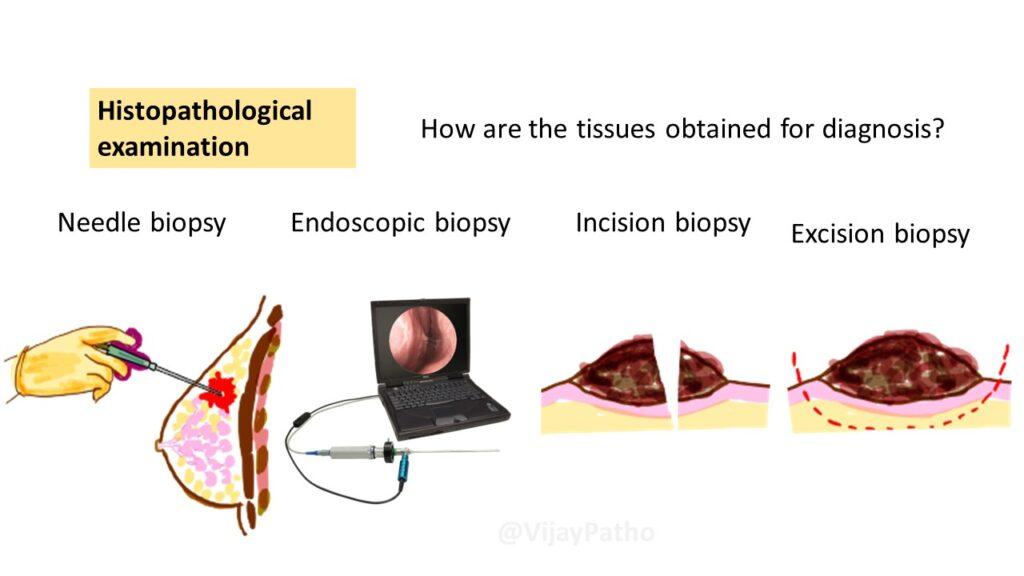
Pathologists examine these tissue samples under a microscope to identify specific cellular and architectural characteristics associated with different types of cancer.
Histopathological examination helps provide an accurate diagnosis, determine tumor grade and stage, and guide treatment decisions.
What is immunohistochemistry (IHC) and how does it contribute to cancer diagnosis?
Immunohistochemistry (IHC) is a specialized laboratory technique used in cancer diagnosis that helps detect specific proteins or markers in tissue sections. By using antibodies that recognize and bind to these proteins, IHC allows pathologists to visualize the presence or absence of certain markers on cancer cells. This information aids in determining the tumor’s characteristics, such as its molecular subtype, hormone receptor status, or the expression of specific biomarkers. IHC plays a crucial role in distinguishing between different types of tumors, guiding treatment decisions, and providing prognostic information.
For example, in breast cancer, immunohistochemistry can detect the presence of estrogen receptors (ER), progesterone receptors (PR), and human epidermal growth factor receptor 2 (HER2). This information is crucial for determining the appropriate treatment approach, such as hormone therapy or targeted therapy with HER2 inhibitors.
Immunohistochemistry provides valuable insights into the nature of the tumor, its potential aggressiveness, and the likelihood of response to specific treatments. It helps in distinguishing between different types of tumors, identifying prognostic markers, and guiding personalized treatment decisions.
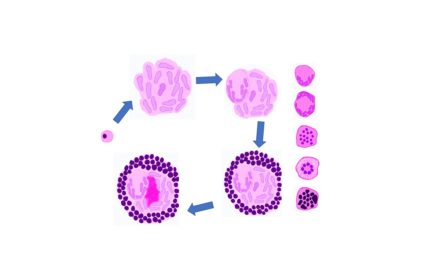
What is flow cytometry and how does it aid in cancer diagnosis?
Flow cytometry is a sophisticated laboratory technique used to analyze individual cells. It involves labeling cells with fluorescently-labeled antibodies that target specific proteins or markers present on the cell surface. By passing the labeled cells through a flow cytometer, the instrument can detect and measure the fluorescence emitted by each cell.
Flow cytometry can provide information about the presence of specific markers, assess cell proliferation, analyze DNA content, and identify different cell populations. In the context of cancer diagnosis, flow cytometry is particularly useful in diagnosing and classifying hematological malignancies, such as leukemia and lymphoma.
What are molecular techniques and how do they contribute to cancer diagnosis?
Molecular techniques, including Polymerase Chain Reaction (PCR), Fluorescence In Situ Hybridization (FISH), and Next-Generation Sequencing (NGS), play a vital role in cancer diagnosis.
PCR amplifies specific DNA sequences, allowing for the detection of genetic mutations or rearrangements associated with cancer.
FISH uses fluorescently-labeled DNA probes to identify specific genetic abnormalities, such as gene amplifications or translocations.
NGS enables the sequencing of large amounts of DNA or RNA, providing detailed information about genetic mutations, gene expression patterns, and genomic alterations.
These molecular techniques help identify specific genetic changes in cancer cells, determine prognosis, guide treatment decisions, and monitor treatment response.
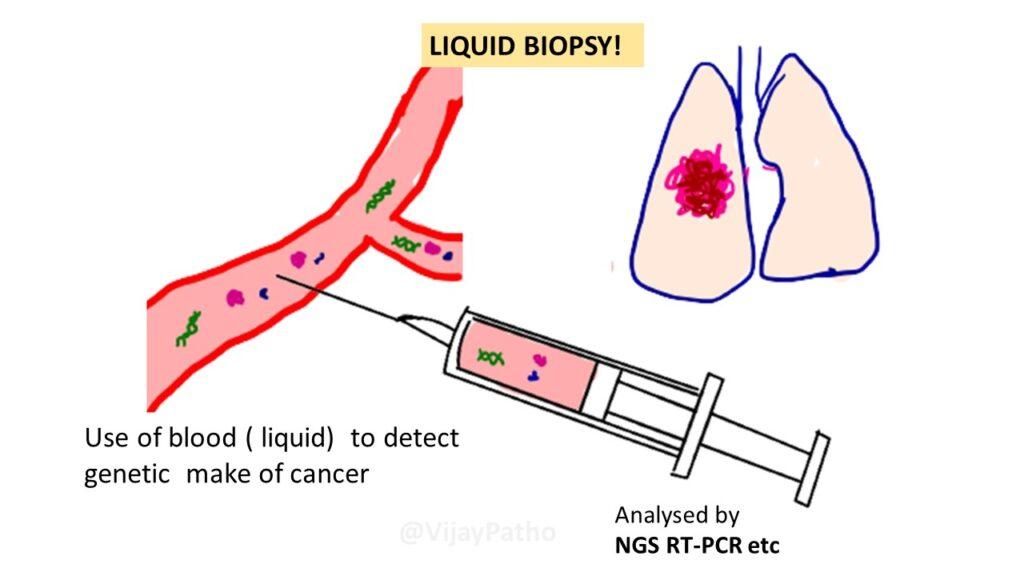
What is liquid biopsy and how does it contribute to cancer diagnosis?
Liquid biopsy is an emerging non-invasive technique in cancer diagnosis. It involves the analysis of circulating tumor components, such as circulating tumor cells (CTCs) and cell-free DNA (cfDNA), in the blood or other body fluids. Liquid biopsy provides valuable information about tumor characteristics, genetic mutations, and treatment response. It can be particularly useful when tissue biopsy is challenging or not feasible, such as in metastatic cancer
How do tumor markers contribute to cancer diagnosis?
Tumor markers are substances found in the blood, urine, or other body fluids of some cancer patients. They can provide additional information about the presence and behavior of cancer cells. While elevated levels of tumor markers can suggest the presence of cancer, they are not definitive diagnostic tests and should be used in conjunction with other diagnostic methods and medical evaluation for accurate diagnosis and treatment decisions. Read more CLICK HERE
What are the imaging techniques used in cancer diagnosis?
Imaging techniques are an essential part of cancer diagnosis as they provide non-invasive visualization of the internal structures of the body. Common imaging techniques used in cancer diagnosis include X-ray, computed tomography (CT), magnetic resonance imaging (MRI), positron emission tomography (PET), and ultrasound.
How does each imaging technique contribute to cancer diagnosis?
X-ray: Provides images of bones and can help identify bone tumors or lung tumors.
CT: Creates detailed cross-sectional images, aiding in visualizing solid tumors, evaluating lymph node involvement, and guiding interventional procedures.
MRI: Uses magnetic fields and radio waves to generate detailed images, offering excellent soft tissue visualization and helping detect and characterize tumors in various organs.
PET: Involves injecting radioactive material to detect areas of increased glucose metabolism, useful for detecting and staging cancers, assessing treatment response, and detecting recurrent disease.
Ultrasound: Uses sound waves to create images and is particularly useful in imaging solid organs, aiding in tumor detection, evaluation, and guiding interventional procedures.
In summary, imaging techniques play a crucial role in cancer diagnosis. X-ray, CT, MRI, PET, and ultrasound provide valuable information about the presence, characteristics, and extent of tumors. They aid in treatment planning, monitoring treatment response, and detecting cancer recurrence. The choice of imaging technique depends on the specific clinical scenario and the type of cancer being evaluated.
By combining these laboratory methods and imaging techniques, healthcare professionals can make accurate cancer diagnoses, understand tumor characteristics, and develop personalized treatment plans for patients.
Remember, early detection and timely diagnosis are crucial in improving cancer outcomes. Regular screenings, thorough physical examinations, and appropriate utilization of laboratory methods can significantly contribute to the effective management of cancer and ultimately improve patient outcomes.
Click here to watch the tutorial on Lab diagnosis of cancer.




Recent Comments