Carcinoma Stomach: INTESTINAL VS DIFFUSE GASTRIC CANCER
Q: What are the two main types of gastric cancer?
A: The two main types of gastric cancer are intestinal type and diffuse type.
Q: What causes diffuse type gastric cancer?
A: Diffuse type gastric cancer is primarily caused by the loss of a protein called E-cadherin, which is responsible for cell adhesion. This loss can occur due to mutations in the tumor suppressor gene called cdh1, which encodes E-cadherin. Other causes of E-cadherin loss include hypermethylation and silencing of the cdh1 promoter region.
Q: What is the pathogenesis of gastric cancer?
A: The pathogenesis of gastric cancer involves multiple factors. Let’s discuss the two main types of gastric cancer: intestinal type and diffuse type.
Intestinal type gastric cancer:
Chronic inflammation caused by Helicobacter pylori infection plays a significant role in the pathogenesis of intestinal type gastric cancer.
Over time, this chronic inflammation leads to the development of precursor lesions, including gastric dysplasia and adenomas.
These precursor lesions can further progress to invasive intestinal type gastric cancer.
Specific dietary factors can also contribute to the development of intestinal type gastric cancer.
Diffuse type gastric cancer:
The key mechanism in diffuse type gastric cancer is the loss of a protein called E-cadherin.
E-cadherin is responsible for cell adhesion, helping cells attach to one another.
Loss of E-cadherin results in the dissociation of cells.
This loss can occur due to mutations in the tumor suppressor gene called cdh1, which encodes E-cadherin.
Additionally, hypermethylation and silencing of the cdh1 promoter region can also lead to the loss of E-cadherin.
The loss of E-cadherin in diffuse type gastric cancer causes the infiltration of tumor cells throughout the gastric wall.
This infiltration evokes a desmoplastic response, leading to stiffening of the stomach wall.
The affected areas show diffuse rugal flattening and a rigid, thickened appearance resembling a leather bottle (linitis plastica) on imaging.
It’s important to note that diffuse type gastric cancer usually occurs sporadically, while intestinal type gastric cancer can be associated with H. pylori infection and specific dietary factors. Familial cases of gastric cancer are more commonly of the diffuse type.
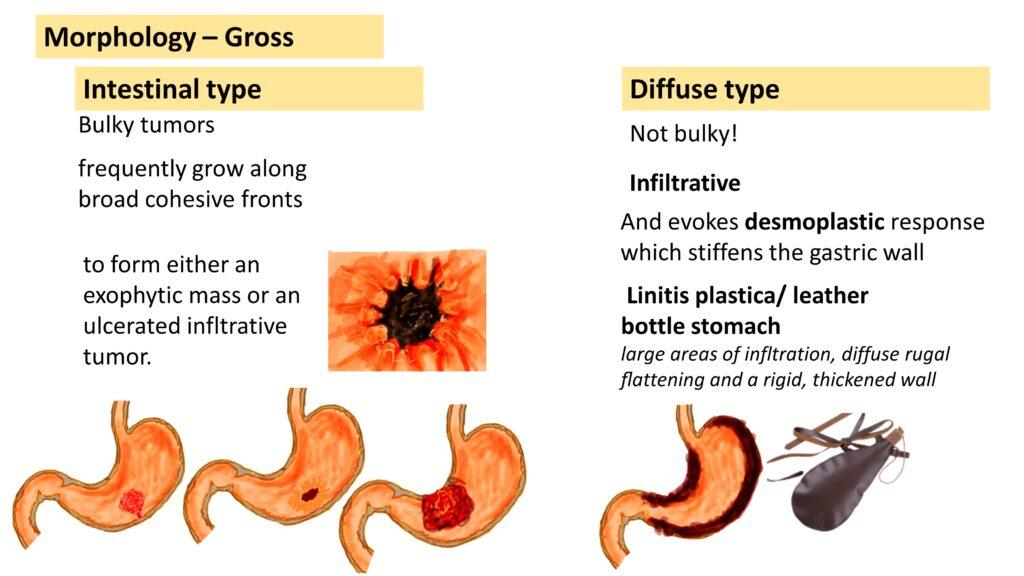
Q: How do intestinal and diffuse type gastric cancers differ in appearance?
A: Intestinal type gastric cancers are often bulky tumors that can form an exophytic mass (protruding growth) or an ulcerated infiltrative tumor. Diffuse type gastric cancers, on the other hand, are characterized by infiltrative growth patterns, causing a rigid and thickened stomach wall. This appearance is often described as “linitis plastica” or “leather bottle” stomach.
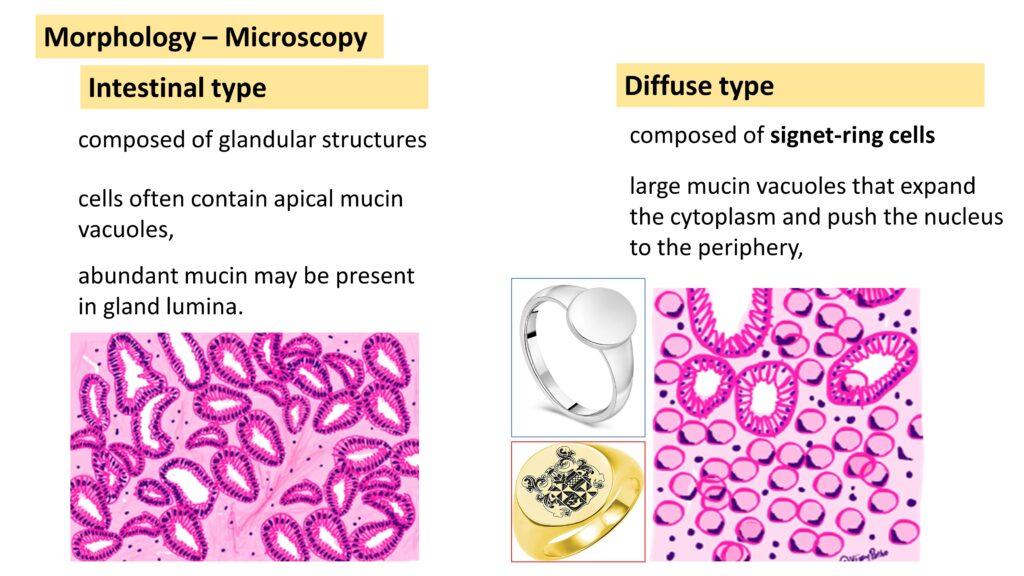
Q: What are the cellular characteristics of intestinal and diffuse type gastric cancers?
A: Intestinal type gastric cancers consist of glandular structures, with cells that frequently contain apical mucin vacuoles. Diffuse type gastric cancers are primarily composed of signet ring cells. These cells have large mucin vacuoles that displace the nucleus to the periphery, giving them a characteristic signet ring appearance.
Q: How do the symptoms of intestinal and diffuse type gastric cancers differ?
A: The early symptoms of both types of gastric cancer may resemble chronic gastritis or peptic ulcer disease, including dyspepsia, dysphagia, and nausea. However, diffuse type gastric cancers are often diagnosed at more advanced stages, leading to additional symptoms such as weight loss, anorexia, early satiety, anemia, and gastrointestinal bleeding.
Q: What are the factors associated with intestinal and diffuse type gastric cancers?
A: Intestinal type gastric cancer is commonly associated with Helicobacter pylori infection, certain dietary factors (e.g., high salt intake, smoked foods), and precursor lesions like gastric dysplasia and adenomas. In contrast, diffuse type gastric cancer has no clear association with H. pylori infection or dietary factors, and it lacks identifiable precursor lesions.
Q: What are the important prognostic indicators for gastric cancer?
A: The depth of tumor invasion into the gastric wall and the extent of nodal and distant metastasis are important prognostic indicators for gastric cancer. Advanced stages of gastric cancer often involve metastasis to regional lymph nodes and distant sites.
Q: Where can gastric cancer metastasize to?
A: Gastric cancer can metastasize to regional lymph nodes, as well as distant sites. Distant metastases can occur in the supraclavicular lymph nodes (known as Virchow’s node), peri-umbilical lymph nodes (Sister Mary Joseph nodules), ovaries (resulting in Krukenberg tumors), left axillary lymph nodes, and the pouch of Douglas.
Q: What is the preferred treatment for gastric cancer?
A: Surgery is the preferred treatment approach for gastric cancer whenever feasible. The goal is to remove the tumor and surrounding affected tissues. In cases where the cancer is advanced and surgery is not possible, treatment options include chemotherapy, radiation therapy, and palliative care to manage symptoms and improve quality of life.
Q: What is the five-year survival rate for gastric cancer?
A: For early gastric cancers that can be completely removed by surgery, the five-year survival rate is generally high, exceeding 90%. However, for advanced cases where the cancer has spread extensively, the five-year survival rate drops to less than 30%.
The table below provides a simplified overview of the differences between the two types of gastric cancer.
| Intestinal Type Gastric Cancer | Diffuse Type Gastric Cancer | |
|---|---|---|
| Pathogenesis | Associated with H. pylori infection and chronic inflammation | Loss of E-cadherin protein leading to cell dissociation |
| Precursor Lesions | Can develop from gastric dysplasia and adenomas | No identified precursor lesions |
| Morphology | Bulky tumors with cohesive growth along broad front, often exophytic or ulcerated | Infiltrative tumors evoking desmoplastic response, resulting in stiffening of gastric wall (leather bottle appearance) |
| Microscopic Features | Glandular structures with apical mucin vacuoles | Signet ring cells with large mucin vacuoles pushing the nucleus to the periphery |
| Age of Presentation | Usually in elderly individuals (around 55 years) | Can occur in younger individuals |
| Gender Predilection | More common in males | Similar prevalence in males and females |
| H. pylori Association | Often associated with H. pylori infection | No significant association with H. pylori |
| Dietary Factors | Specific dietary factors may contribute to pathogenesis | No significant role of dietary factors |
| Incidence Trend | Decreasing incidence in recent years | Incidence remains stable |
| Prognostic Indicators | Depth of invasion and extent of nodal and distant metastasis | Depth of invasion and extent of nodal and distant metastasis |
| Treatment Approach | Surgery remains the preferred treatment whenever possible | Chemotherapy, radiation therapy, and palliative care in advanced cases |
| Five-Year Survival Rate | >90% for early gastric cancers amenable to surgical resection | <30% for advanced gastric cancers |
Please click here to watch the video tutorial of the same



Recent Comments