Ulcerative Colitis
Ulcerative colitis is a inflammatory bowel disease that affects the colon and rectum.
Unlike Crohn disease, ulcerative colitis does not affect the other parts of gastro-intestinal tract.
Extra-intestinal manifestations:
The extra-intestinal manifestations are seen in both the inflammatory bowel diseases.
They include
Migratory polyarthritis
Uveitis
Sacroiliitis
Ankylosing spondylitis
Skin lesions
Primary sclerosing cholangitis
Morphology – Gross
Always involves the rectum and extends proximally
The involvement is continuous. There are no skip lesions in ulcerative colitis like we see in Crohn disease.
Proctitis: refers to involvement of only rectum.
Proctosigmoiditis: refers to involvement of rectum and sigmoid colon
Pancolitis: refers to involvement of entire colon.
Toxic megacolon: refers to Colonic dilation caused by severe disease with inflammation of muscularis propria and neuromuscular dysfunction.
There is a sharp demarcation between the involved and normal mucosa.
The involved mucosa appears red and granular or shows extensive ulceration.
Pseudopolyps: Within the ulcerated mucosa, there can be islands of regenerating mucosa which bulge above the level of ulcerated mucosa. These are known as Pseudopolyps.
Mucosal bridges: The regenerating mucosa overlying the tips of pseudopolyps may fuse to form mucosal bridges.
The thickness of colon wall that is involved in ulcerative colitis is limited to mucosa most often with submucosal involvement at times. This is in contrast to Crohn disease where the entire wall thickness i.e transmural involvement is seen.
Due to the superficial inflammation in ulcerative colitis, there is no wall thickening, no stricture formation or no fistula.
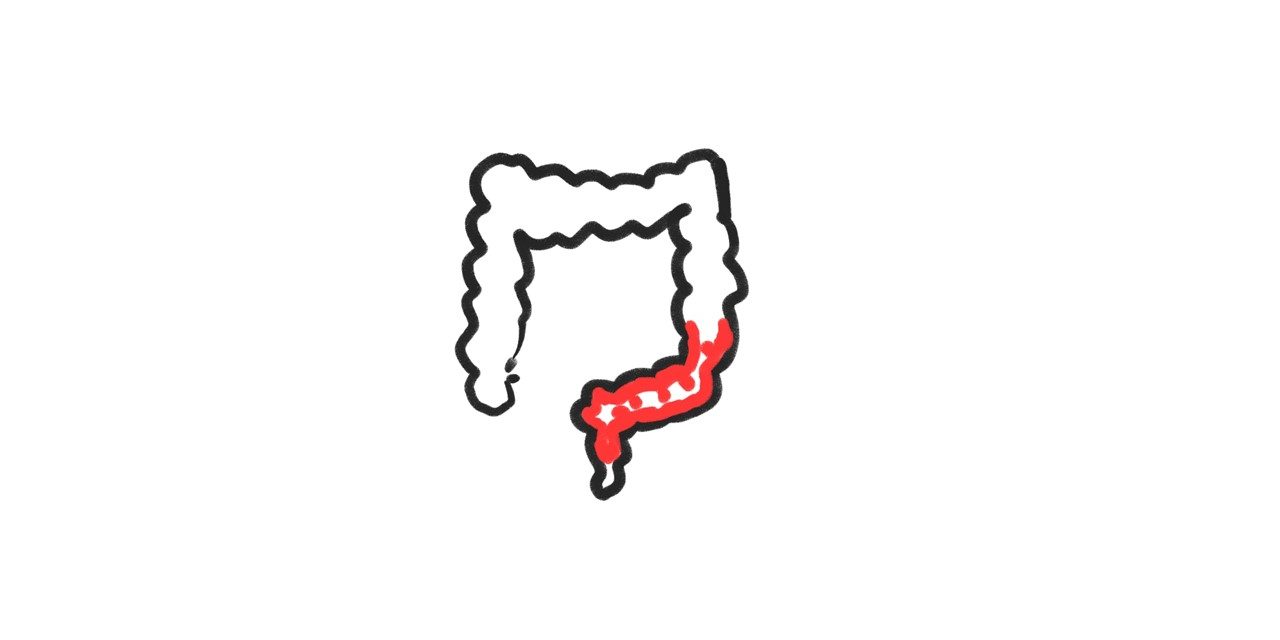
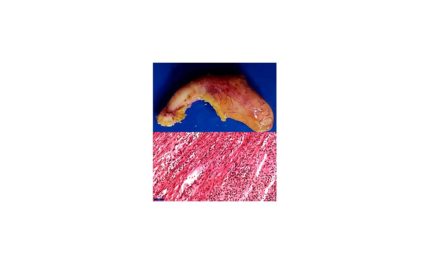
Morphology – Microscopy
The histological features include cryptitis, crypt abscesses and basal plasmacytosis.
Cryptitis: neutrophils infiltrating the lining epithelium of glands or crypts.
Crypt abscess: neutrophils within the glandular lumen.
Basal plasmacytosis: increased number of plasma cells at the base of crypts.
The inflammation is superficial involving the mucosa and superficial submucosa only. Deeper layers are not affected in ulcerative colitis.
Clinical features and treatment
This disease is relapsing and episodic. The episode may last for days to weeks or at times months.
The symptoms include abdominal pain, cramps, diarrhoea, blood in stools (hematochazia), and stringy mucous in stools.
Treatment includes surgical and medical modality. With the availability of better drugs, the incidence of colectomy in ulcerative colitis has reduced.
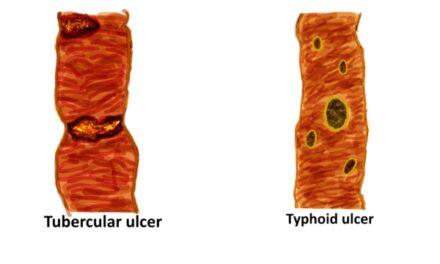
Differences between Crohn disease and Ulcerative colitis.