Type I Hypersensitivity reaction.
What are hypersensitivity reactions?
Hypersensitivity reactions are injurious immune reactions characterized by excessive or harmful reactions of the immune system to antigens.
The antigens can be exogenous from the environment or endogenous self-antigens.
They usually result from an imbalance between effector and regulatory mechanisms, with most often failure in normal regulation being the reason. They are associated with some inherited genetic susceptibility.The mechanisms of tissue injury are the same as effector mechanism except for that they are either excessive, uncontrolled, or misdirected.
Name the types of hypersensitivity reactions.
Type 1 or the Immediate hypersensitivity reaction
Type 2 or the Antibody mediated hypersensitivity reaction
Type 3 or the Immune complex mediated hypersensitivity reaction.
Type 4 or the Cell mediated hypersensitivity reaction.
Describe type 1 hypersensitivity reaction with a neat, labelled diagram.
Type 1 hypersensitivity reaction is triggered by binding of an antigen/ allergen (for example bee sting, peanut, pollen, etc) to IgE antibody on the mast cell surface, in a previously sensitized host. It is a rapid immunologic reaction.
The two phases of type 1 hypersensitivity reactions are as follows:
1. Immediate reaction – this phase is characterized by vasodilation, smooth muscle spasm, vascular leakage, glandular secretions, within minutes of exposure to the allergen.
2. Late phase – this phase is characterized by infiltration of tissues with eosinophils, neutrophils, basophils, monocytes, and CD4 T cells with tissue destruction. This phase sets in about 2 to 24 hours later, without any additional exposure to antigen. This phase may last for several days.
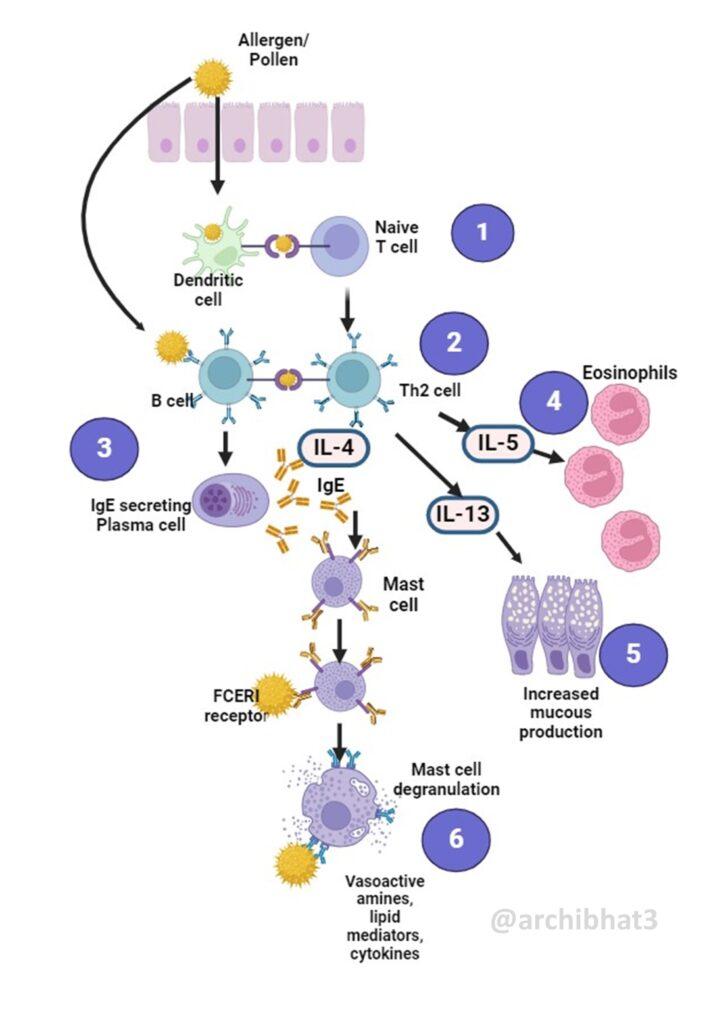
Steps involved in Type 1 Hypersensitivity reaction are as illustrated below
1. Presentation of antigen to the naïve T cells by dendritic cells. Only some antigens can elicit a strong Th2 response.
2. Th2 cells produce cytokines IL-4, IL-5 and IL-13, on encounter with the allergen.
3. IL-4 acts on B cells to stimulate class switching to IgE and promotes the production of more Th2 cells.
4. IL-5 causes development and activation of eosinophils.
5. IL-13 stimulates mucous secretion and increases the production of IgE.
6. IgE bind to the IgE Fc receptors on mast. When these IgE coated mast cells are exposed to the same antigen, the cell is activated and results in release of the mediators by degranulation.
CLICK HERE to read Type II Hypersensitivity reaction