ASTROCYTOMAS: Pilocytic Astrocytoma
What is an Astrocytoma?
- Astrocytomas are the most common glioma and can occur in most parts of the brain and sometimes in the spinal cord
- Originate in astrocytes, a particular kind of glial cells which are star-shaped brain cells in the cerebrum (Figure 1)
- Astrocytomas do not usually spread outside the brain and spinal cord and does not usually affect other organs
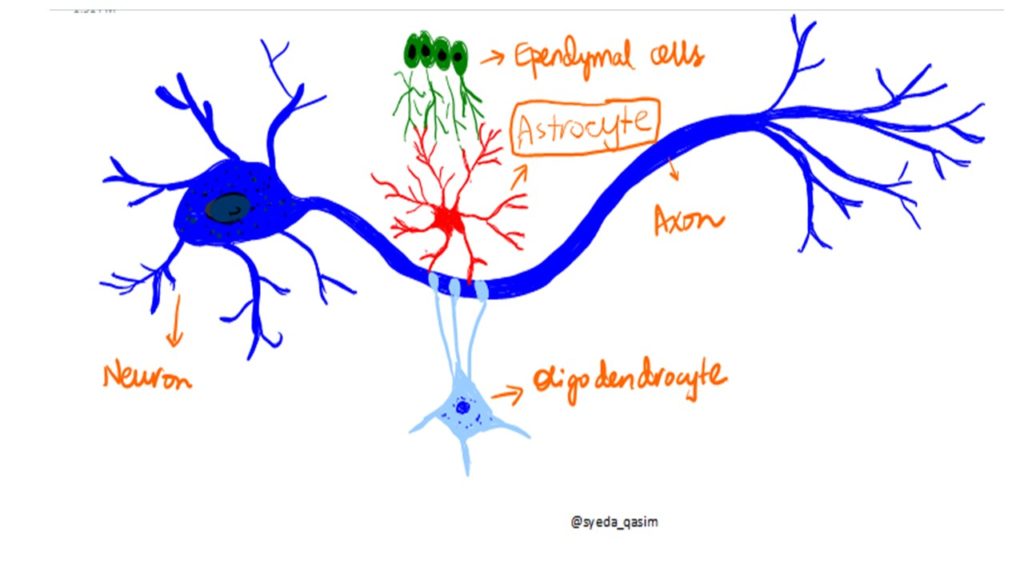
Figure 1: Origin of Astrocytoma
General Classification:
- Narrow zones of infiltration (mostly noninvasive tumors; e.g., pilocytic astrocytoma, pleomorphic xanthoastrocytoma), that often are clearly outlined on diagnostic images
- Diffuse zones of infiltration (e.g., high-grade astrocytoma, glioblastoma [CLICK HERE] ), that can arise at any location in the central nervous system, but with a preference for the cerebral hemispheres; usually occur in adults, and have a tendency to progress to more advanced grades
Epidemiology:
- People can develop astrocytomas at any age
- The low-grade type is more often found in children or young adults, while the high-grade type is more prevalent in adults.
- Astrocytomas in the base of the brain are more common in young people and account for roughly 75% of neuroepithelial tumors
PILOCYTIC ASTROCYTOMA
- Pilocytic means “hair-like,” due to long, bipolar processes
- Most common CNS neoplasm of childhood
- Occurs more often in children and young adults (in the first 20 years of life)
- Originate in the cerebellum, near the brainstem, in the hypothalamic region, or the optic chiasm, but may occur in any area where astrocytes are present, including the cerebral hemispheres and the spinal cord
- Usually slow growing and benign
- The neoplasms are associated with the formation of one or more cysts, and can become very large and well-circumscribed
- Better prognosis than diffuse types, particularly if resectable (such as cerebellar tumors)
Epidemiology:
- Juvenile pilocytic astrocytoma occurs at a rate of 2 in 100,000 people with most affected are children ages 5–14 years
- Astrocytomas account for 50% of pediatric primary central nervous system tumors. About 80-85% of cerebellar astrocytomas are juvenile pilocytic astrocytomas
Associations:
- Juvenile pilocytic astrocytoma is associated with neurofibromatosis type 1 (NF1), and optic gliomas are among the most frequently encountered tumors in patients with this disorder
Symptoms:
- The most common symptoms are associated with increased intracranial pressure due to the size of the neoplasm
- Failure to thrive, headache, nausea, vomiting, irritability, torticollis, difficulty to coordinate movements, and nystagmus are other symptoms
Gross & Microscopic description:
- Macroscopically, an astrocytoma is a mass that looks well-circumscribed and has a large cyst. The neoplasm may also be solid
- Histologically there are bipolar cells with long “hair like” GFAP-positive processes, giving the name “pilocytic” (Figure 2)
- Presence of Rosenthal fibers (tapered corkscrew shaped, brightly eosinophilic, hyaline masses)
- Also eosinophilic granular bodies, and microcysts may be present
- Myxoid foci and oligodendroglioma-like cells may also be present Long-standing lesions may show hemosiderin-laden macrophages and calcifications
Figure 2: Histological Appearance of Pilocytic Astrocytoma
What are the positive stains?
- GFAP
- PTAH
- PAS (protein droplets), alpha-1-antichymotrypsin (protein droplets)
Treatment:
- Surgical removal, however total resection is often not possible.
- Location could prohibit access to the neoplasm and lead to incomplete or no resection at all
- Removal of the tumor will generally allow functional survival for many years
- If surgery is not possible chemotherapy or radiation is used

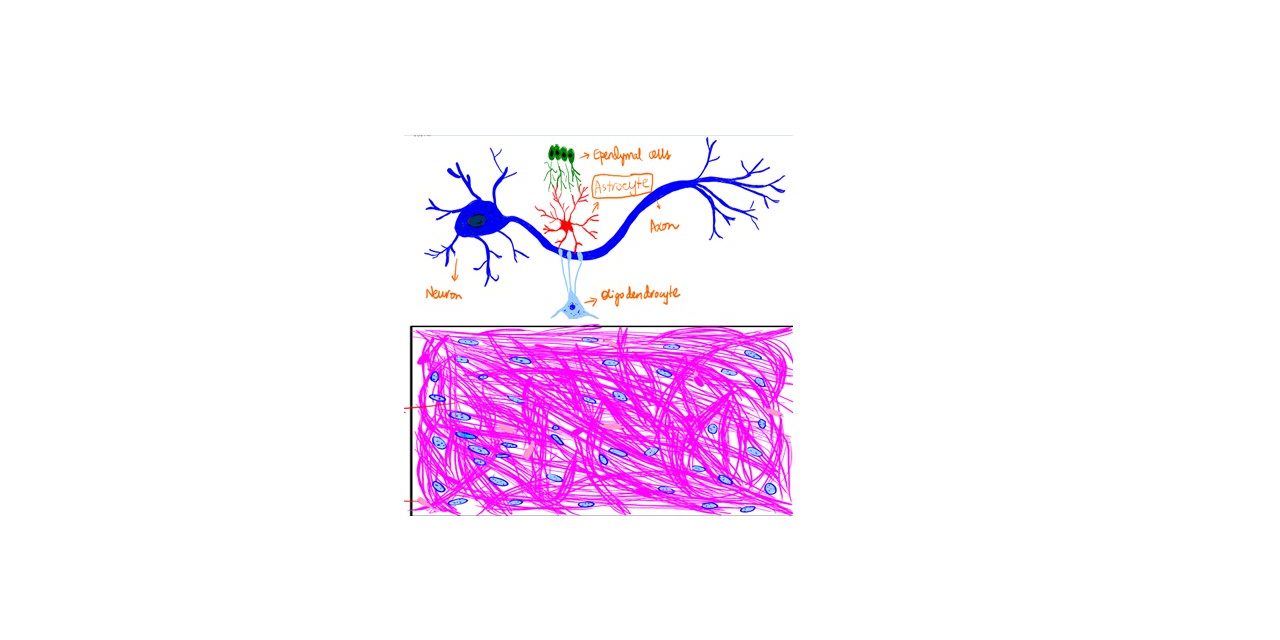
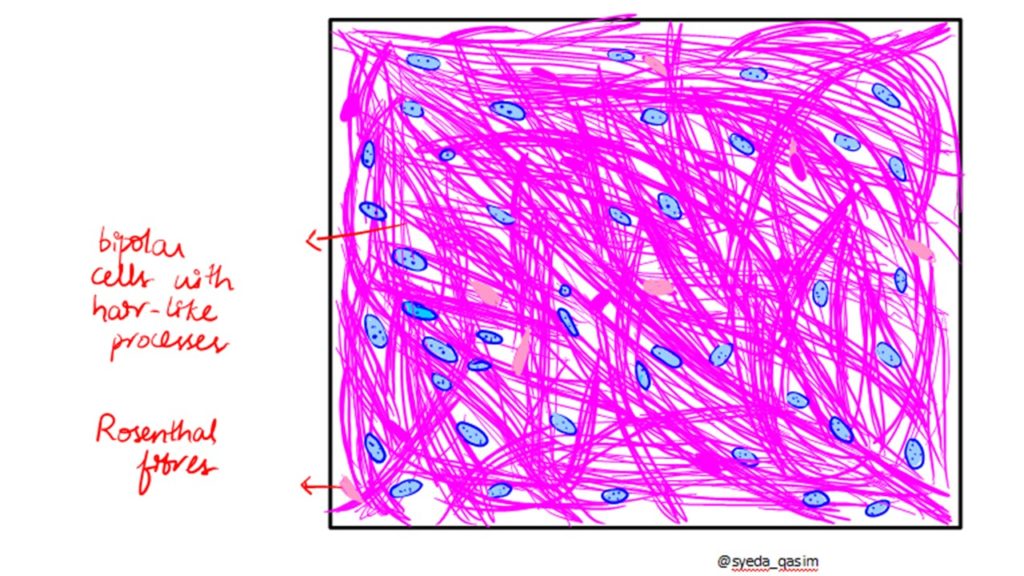 Figure 2: Histological Appearance of Pilocytic Astrocytoma
Figure 2: Histological Appearance of Pilocytic Astrocytoma