Thalassemia
Genetically heterogeneous disorder caused by germline mutations that reduce -globin or -globin synthesis, which leads to anemia, tissue hypoxia, and red cell hemolysis. All the manifestations are Related to the imbalance in globin chain synthesis.
Thalassa means “sea” in Greek. it is more common in Mediterranean basin where it is endemic. Also seen in Middle East, tropical Africa, the Indian subcontinent, and Asia. It has Middle East, tropical Africa, the Indian subcontinent, and Asia.
It has Autosomal recessive inheritance Which means, if both the parents are carriers, then 25% of the offsprings are diseased and 50% will be carriers
Thalassemia is further divided into
α Thalassemia – deficient synthesis of α globin chains.
β Thalassemia – deficient synthesis of β globin chains.
The major consequences of thalassemia are due to two imprtant reasons
1. Hemoglobin deficiency– due to deficient synthesis of α or beta chains.
2. Relative excess of the other globin chain– resulting in precipitation which causes destruction of RBC precursors.
α Thalassemia
is due to deficient synthesis of α globin chains.
Molecular pathogenesis.
the genes for α globin chain is present on chromosime 16. they are in pairs i.e each chromosome 16 has a pair of α genes, so total of 4 genes are present ( as we have 2 chromosomes)
Deletions involving alpha gene loci in one or more genes( Of the 4 genes)α thalassemia. the types are as below
αα/ αα – Normal
– α/ αα : Silent Carrier State
– – / αα OR α -/ α- : α-Thalassemia Trait
– -/ – α : Hemoglobin H (HbH) Disease.
– -/ – – : Hydrops Fetalis.
Clinical features :
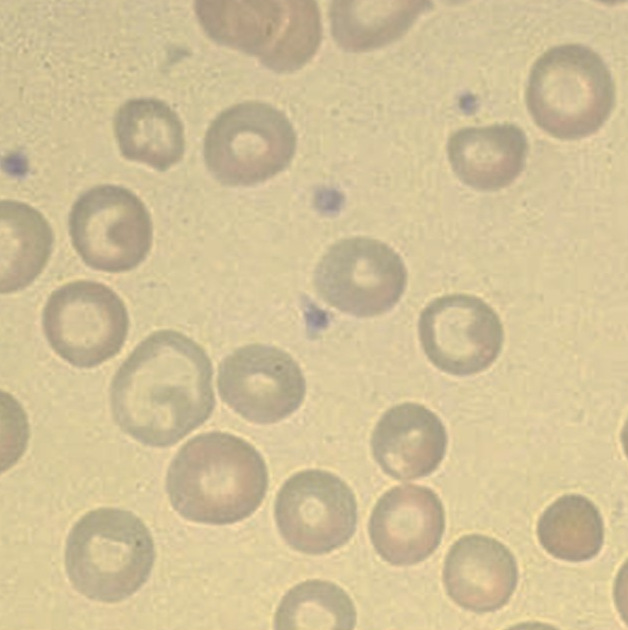
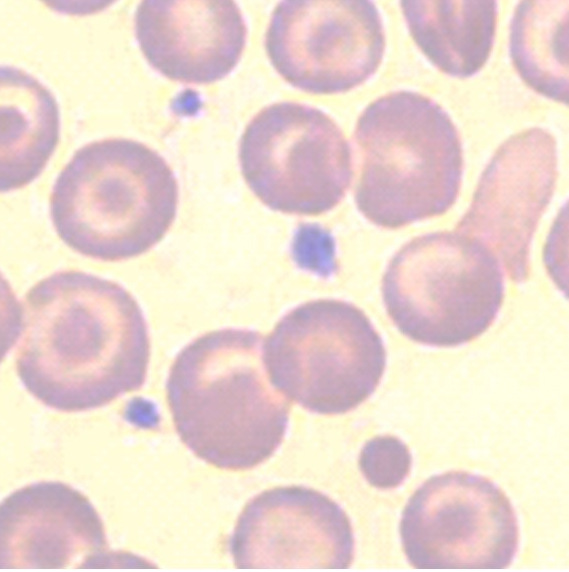
– α/ αα : Silent Carrier State: These individuals have barely detectable reduction in α-globin chain synthesis. Often Asymptomatic. Mild microcytosis seen on peripheral smear
– – / αα OR α -/ α- : α-Thalassemia Trait:
Both genotypes produce similar deficiencies of α-globin, they have minimal or no anemia, and no abnormal physical signs.Microcytosis seen on peripheral smear. HbA2 levels are normal or low.
– -/ – α : Hemoglobin H (HbH) Disease.
Most common in Asian populations.
The relatively excess beta globin chain precipitate as β4 tetramers ( HbH ). These β4 tetramers ( HbH ) have extremely high affinity for oxygen resulting in tissue hypoxia tissue hypoxia, which is frequently exaggerated compared to haemoglobin levels
β4 tetramers also are prone to oxidation resulting in precipitation which form inclusions in the red cell.RCS with inclusionsa are sequestered in speen followed by hemolysis by the macrophages.
Thus these patients have Moderately severe anemia
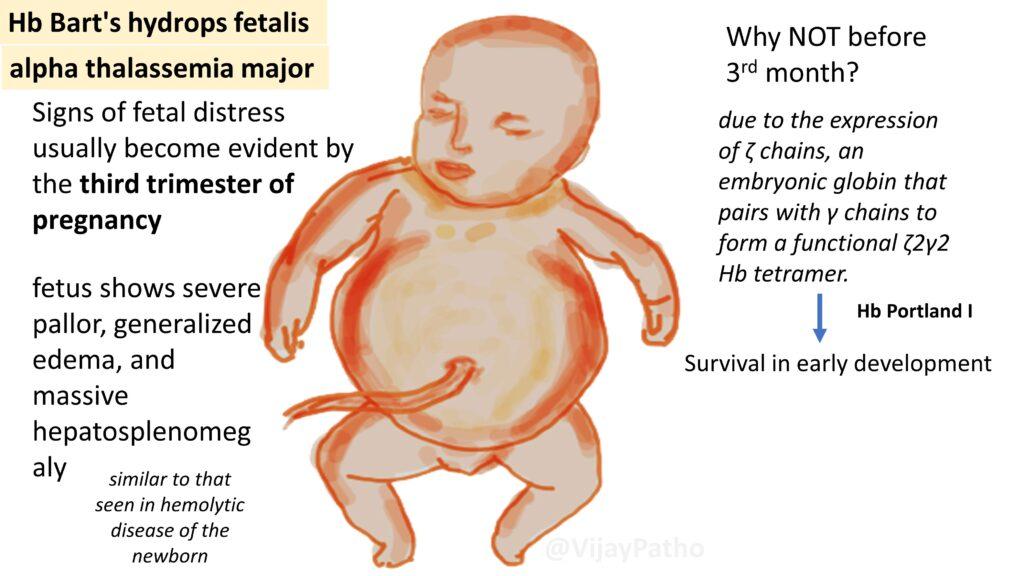
– -/ – – : Hydrops Fetalis. also referred to as alpha thalassemia major
Most severe form .
The relatively excess gamma globin chain precipitate as form γ4 tetramers ( Hb Barts ). they also have extremely high affinity to oxygen resulting in severe tissue hypoxia. Death in utero/ shortly after birth ensues.
if the fetus survives, Signs of fetal distress usually become evident by the third trimester of pregnancy. Survival in early development is mainly due to the expression of ζ chains, an embryonic globin that pairs with γ chains to form a functional ζ2γ2 Hbtetramer.
Fetus shows severe pallor, generalized edema, and massive hepatosplenomegaly. These findings are similar to that seen in hemolytic disease of the newborn. The babies need life long transfusion for survival
Iron overload! is a potential complication.
HSC transplantation – curative
Lab Diagnosis of Alpha Thalassemia
CBC: Mildly decreased hemoglobin
Low MCV & MCH
Mild microcytosis on peripheral smear
Hb electrophoresis & HPLC: HbH and Hb Barts
Molecular testing: Detect the alpha deletion
Treatment
Depends on type: mainly Blood transfusions. Iron chelation therapy if there is iron overload. Avoidance of oxidant drugs is very important.
Click here to watch the video tutorial on alpha thalassemia.




Recent Comments