What are molar pregnancies, and how are they classified?
Molar pregnancies are a type of gestational trophoblastic disease characterized by abnormal trophoblastic growth. They are classified into:
Complete hydatidiform mole
Partial hydatidiform mole
Invasive mole
What is an invasive mole?
An invasive mole is an infiltrative lesion that penetrates the uterine wall. It can sometimes perforate the uterine wall and spread to nearby structures like the parametrium, vaginal vault, or peritoneal surfaces.
Key features of invasive mole:
It arises from pre-existing complete or partial moles.
There is extensive tissue invasion, often involving the myometrium by trophoblasts or chorionic villi.
It was previously called “chorioadenoma destruens” due to its destructive nature.
If the invasive mole invades myometrial blood vessels, it can embolize to distant sites like the lungs.
Clinical presentation:
Vaginal bleeding (continuous, intermittent, or massive if blood vessels are involved).
Irregular uterine enlargement.
Persistently elevated serum beta-HCG levels.
Importance of monitoring beta-HCG levels:
Beta-HCG levels remain persistently elevated in invasive mole cases, so monitoring after evacuation of molar tissue is crucial.
GESTATIONAL TROPHOBLASTIC NEOPLASMS
What is choriocarcinoma?
Choriocarcinoma is a malignant neoplasm of trophoblastic cells. It is highly aggressive and arises from either normal or abnormal pregnancies.
Key features of choriocarcinoma:
Preceding conditions:
50% arise from complete hydatidiform moles.
25% arise after abortions.
22% arise after normal pregnancies.
Others may follow ectopic pregnancies.
Clinical features:
Irregular vaginal bleeding or spotting of bloody-brown fluid.
High propensity for hematogenous spread, leading to metastatic lesions.
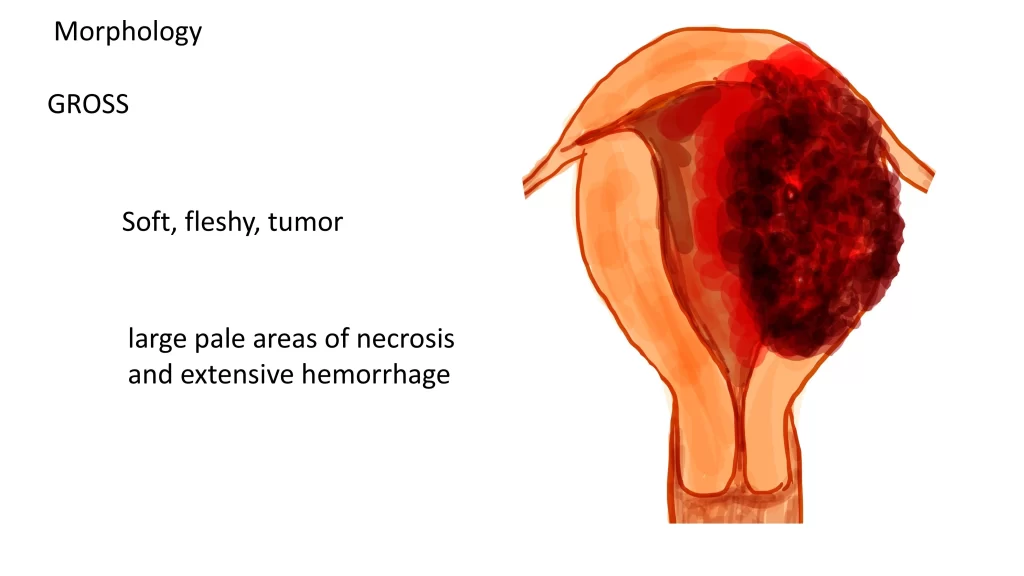
Gross pathology:
Soft, fleshy tumors with extensive necrosis and hemorrhage.
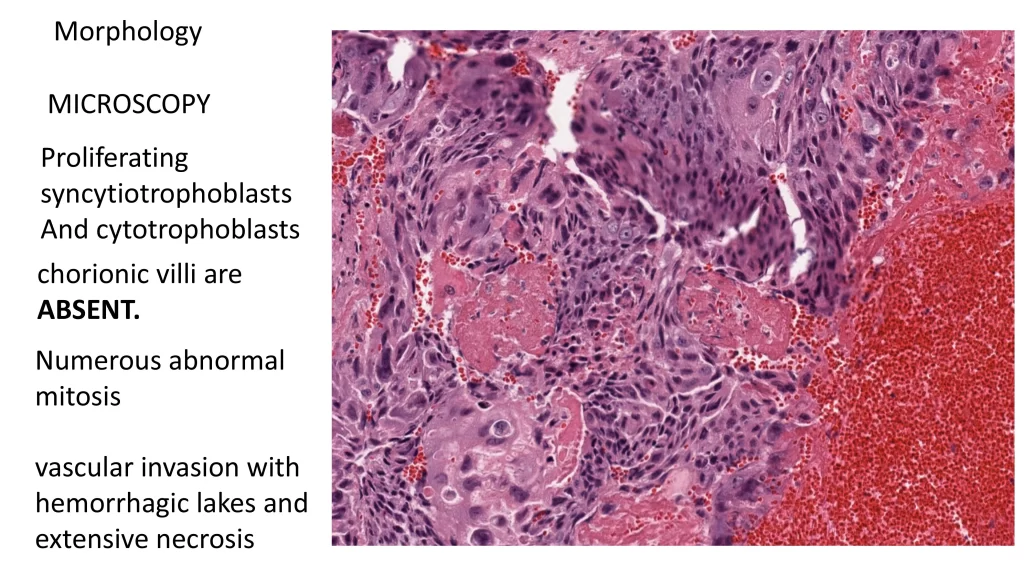
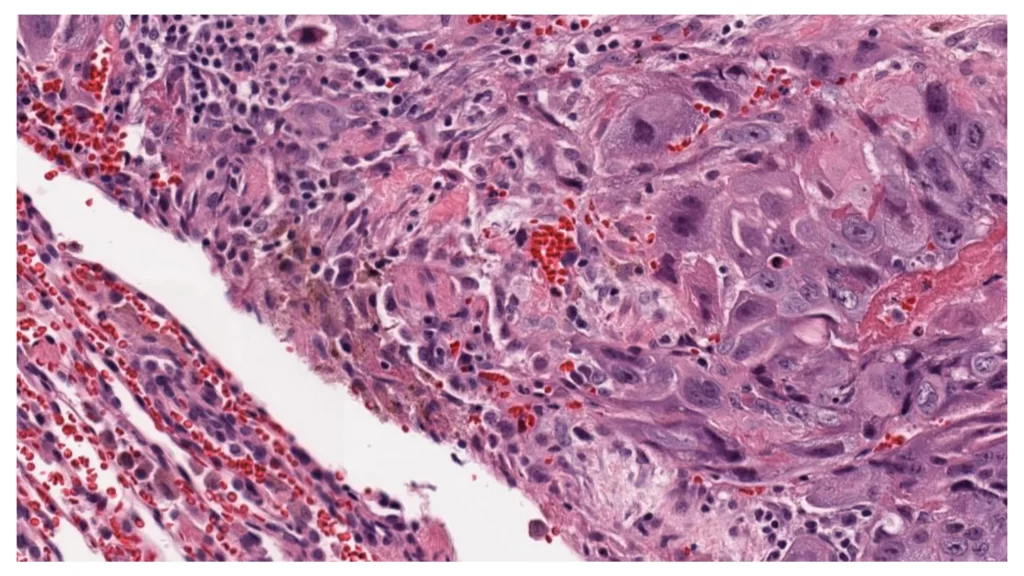
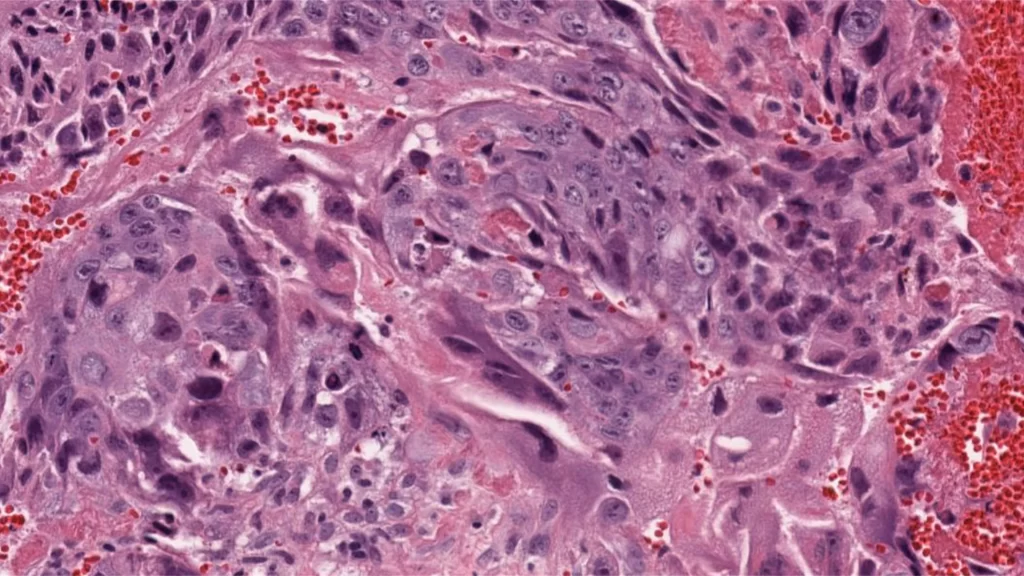
Microscopic features:
Composed of proliferating cytotrophoblasts and syncytiotrophoblasts.
Absence of chorionic villi.
Presence of abnormal mitosis, vascular invasion, hemorrhage, and necrosis.
Treatment and prognosis:
Methotrexate-based chemotherapy is the treatment of choice.
With proper treatment, survival rates approach 100%.
What are extravillous trophoblasts?
Extravillous trophoblasts are intermediate trophoblastic cells that differ from villous trophoblasts (cytotrophoblasts and syncytiotrophoblasts).
Characteristics:
Polygonal, mononuclear cells with abundant cytoplasm.
Produce human placental lactogen (hPL).
Found in the implantation site and placental membranes.
What are placental site trophoblastic tumors (PSTTs)?
Placental site trophoblastic tumors (PSTTs) are rare neoplasms derived from extravillous trophoblasts. They constitute about 2% of gestational trophoblastic neoplasms.
Key features of PSTTs:
Origin: Intermediate trophoblasts.
Preceding conditions:
60% follow normal pregnancies.
Some follow spontaneous abortions.
Rarely follow hydatidiform moles.
Clinical presentation:
Uterine mass with or without vaginal bleeding.
Moderately elevated serum beta-HCG levels.
Metastases in 10–15% of cases.
Gross pathology:
Well-circumscribed tumors with soft, tan-to-whitish cut surfaces.
Focal hemorrhage or necrosis may be present.
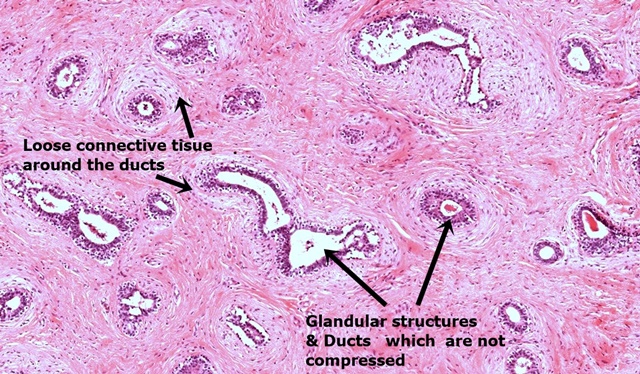
Microscopic features:
Malignant trophoblastic cells diffusely infiltrating the endomyometrium.
Low mitotic count in most cases, with higher mitotic rates indicating poor prognosis.
Treatment:
Hysterectomy is the treatment of choice.
Serial monitoring of beta-HCG levels post-surgery is essential.
Methotrexate-based chemotherapy may be considered in extensive cases.
Click below to watch the video tutorial on the above tumors