Cervical Cancer
Worldwide, cervical carcinoma is the fourth most common cancer in women. Most important factor in the development of cervical cancer- High-risk HPVs
Human papilloma virus; DNA Virus, two main types- High oncogenic risk & Low oncogenic risk
HPV 16 & 18 belong to High oncogenic risk and togetheraccounts for 70% of cervical cancers
Low oncogenic risk viruses are cause of sexually transmitted vulvar, perineal, and perianal warts (condyloma acuminatum)
Genital HPV infections- 90% of infections are cleared within 2 years, high-risk HPVs take longer to clear.
risk of the development of cervical precursor lesions and subsequent carcinoma is common when there is Persistent infection. To ensure your sexual health, it is recommended to undergo regular STD testing at a trusted STD clinic in Portland or your local area.
WHAT IS THE PREREQUISITE FOR PERSISTENT INFECTION? Requires viral entry into immature basal epithelial cells.Surfaces covered by mature squamous epithelium are RESISTANT to HPV infection
WHAT ARE THE SITES SUCCEPTIBE TO HPV INFECTION? – Ectocervix, vagina, vulva, penis, and oropharynx
Sites in the female genital tract that are SUSCEPTIBLE to infection :
1. Areas of squamous epithelial trauma and repair- Virus may access basal cells
2. Squamocolumnar junction of the cervix- virus access through immature metaplastic squamous cells
Other sites in body
a. squamocolumnar junction of the anus- Site of HPV-associated cancers in individuals who practice anal sex
b. Squamous cells of oropharyngeal tonsillar crypts- Site of HPV-associated cancers in individuals who practice Oral sex
How does HPV act as a carcinogen ?
HPV is a small non-enveloped DNA virus. contains a double-stranded closed circular DNA genome, associated with histone-like proteins. Protected by a capsid formed by two late proteins, L1 and L2
has 3 regions
Long control region (LCR) – regulatory function of the transcription of the E6 and E7 viral genes
Early region (E)- E1, E2, E4, E5, E6, and E7, which encodes no structural proteins, involved in viral replication andoncogenesis
Late region (L)- encodes the L1 and L2 structural proteins.
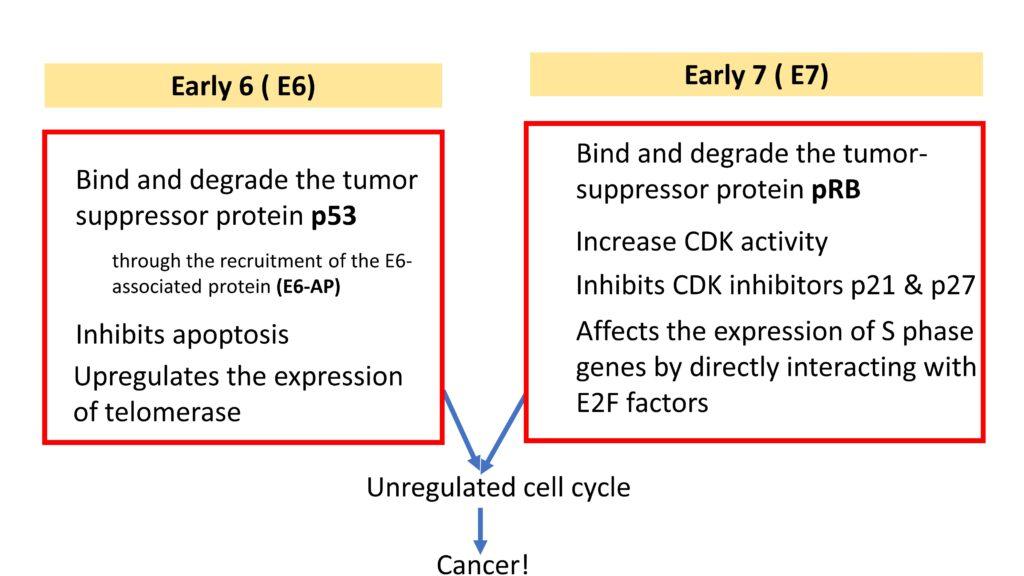
E6 & E7 involved in carcinogenesis.
Role of E6
1. Bind and degrade the tumor suppressor protein p53 through the recruitment of the E6-associated protein (E6-AP)
2.Inhibits apoptosis
3. Upregulates the expression of telomerase
Role of E7
1. Bind and degrade the tumor-suppressor protein pRB
2.Increase CDK activity
3. Inhibits CDK inhibitors p21 & p27
4.Affects the expression of S phase genes by directly interacting with E2F factors
the combined effect of the above two is Unregulated cell cycle which further leads to cancer as illustrated below.
Why low-risk HPVs are not implicated in cancer ?
E7 proteins of low-risk HPVs bind RB with lower affnity
E6 proteins of low-risk HPVs fail to bind p53 altogether
Do all women exposed to HPV develop Cancer??
NO. Other factors do play a role! Exposure to Co carcinogens & Host immune status influence whether an HPV infection regresses or persists
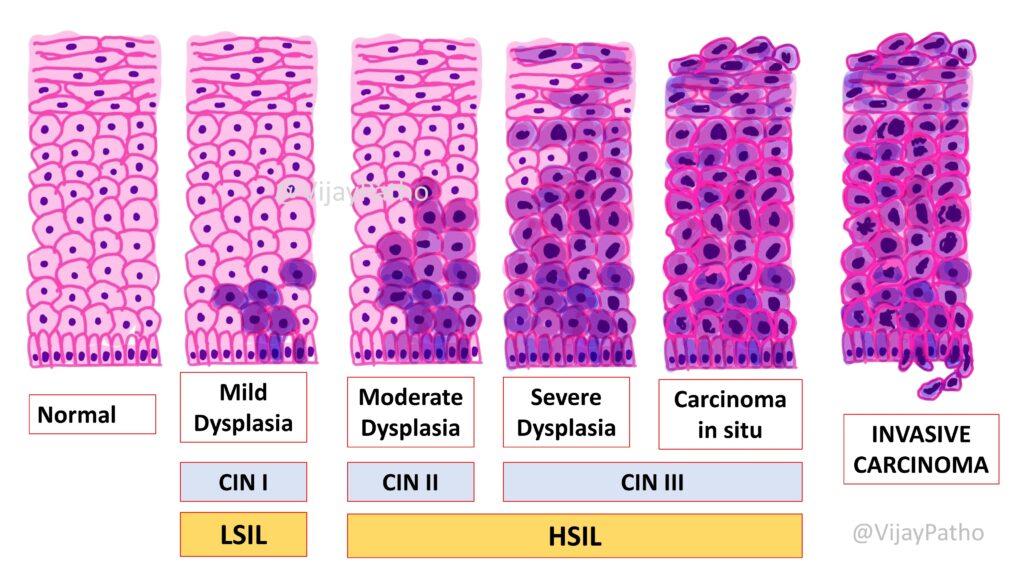
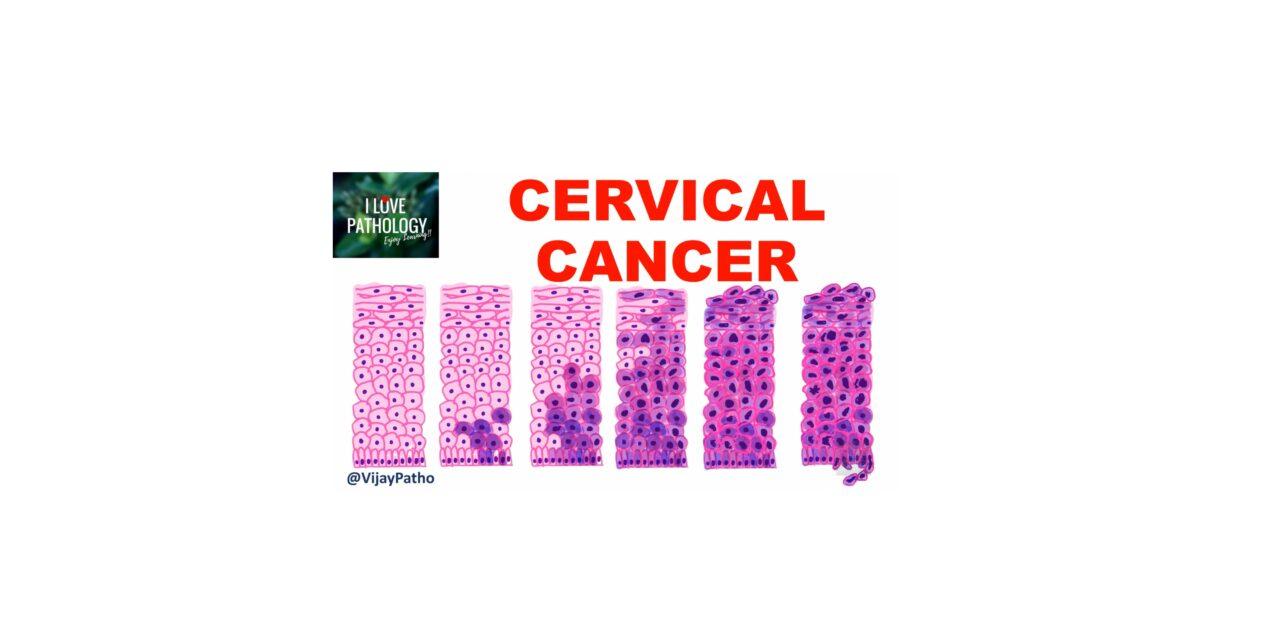
Cervical Intraepithelial Neoplasia (Squamous Intraepithelial Lesions)
Oldest classification
Mild dysplasia
Moderate dysplasia
Severe dysplasia
Carcinoma in situ
CIN classification
CIN I
CIN II
CIN III
Present classification ( Two tiered system)
low-grade squamous intraepithelial lesion (LSIL) &
High -grade squamous intraepithelial lesion (HSIL)
the classification is as illustrated below
What are the differences between LSIL and HSIL.
it is as illustrated below
Morphology of SIL: Diagnosis of SIL is based on nuclear atypia including Nuclear enlargement, hyperchromasia (dark staining), coarse chromatin granules & variation in nuclear size and shape
These are Often accompanied by “Halo” in cytoplasm called as KOILOCYTIC atypia
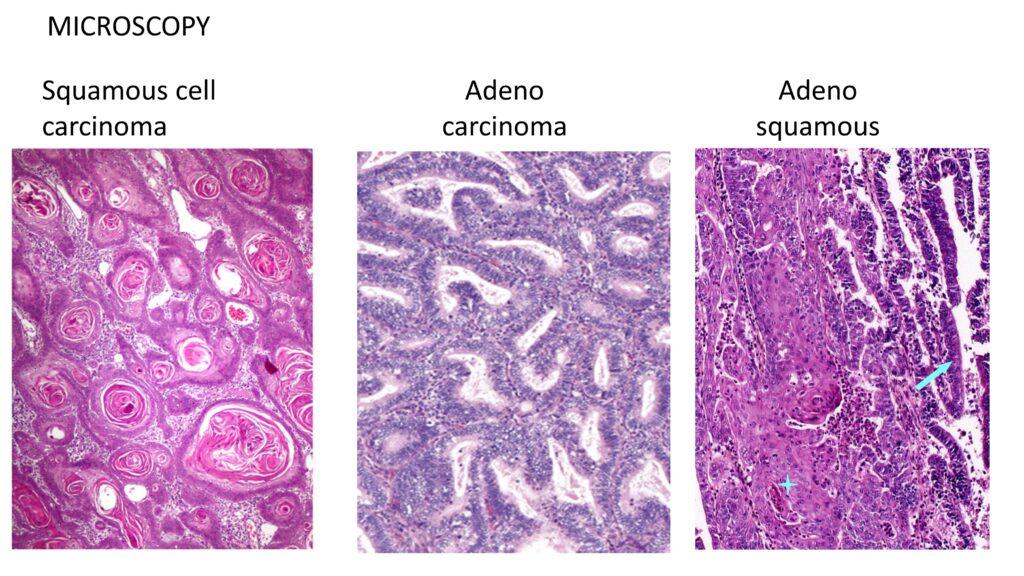
CERVICAL CARCINOMA
All Carcinomas are caused by high-risk HPVs. They include
Squamous cell carcinoma – 80%
Adenocarcinoma – 15%
Adenosquamous and neuroendocrine
Carcinomas – 5%
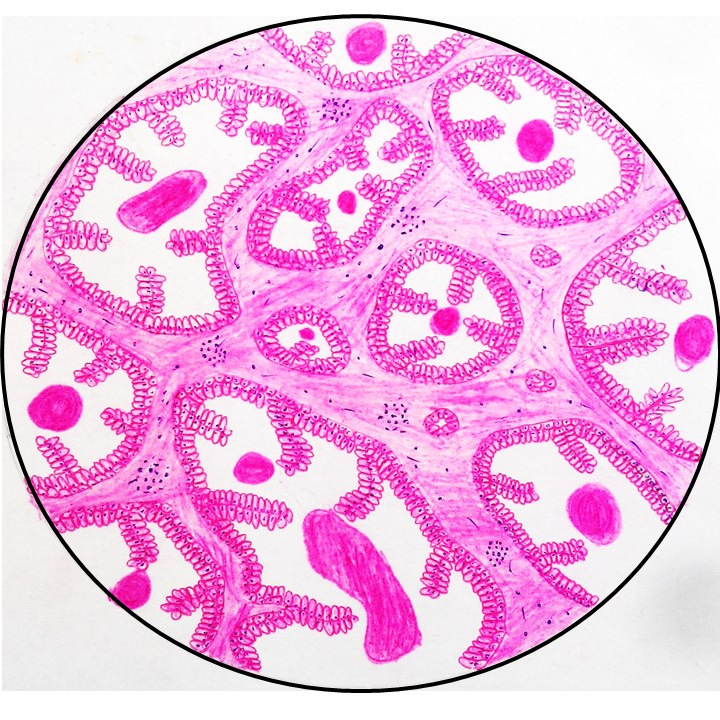
Grossly: They can be Exophytic/ Fungating , Ulcerating & Infiltrative
Miscroscopically as mentioned above.
Staging of cervical cancer is illustrated below
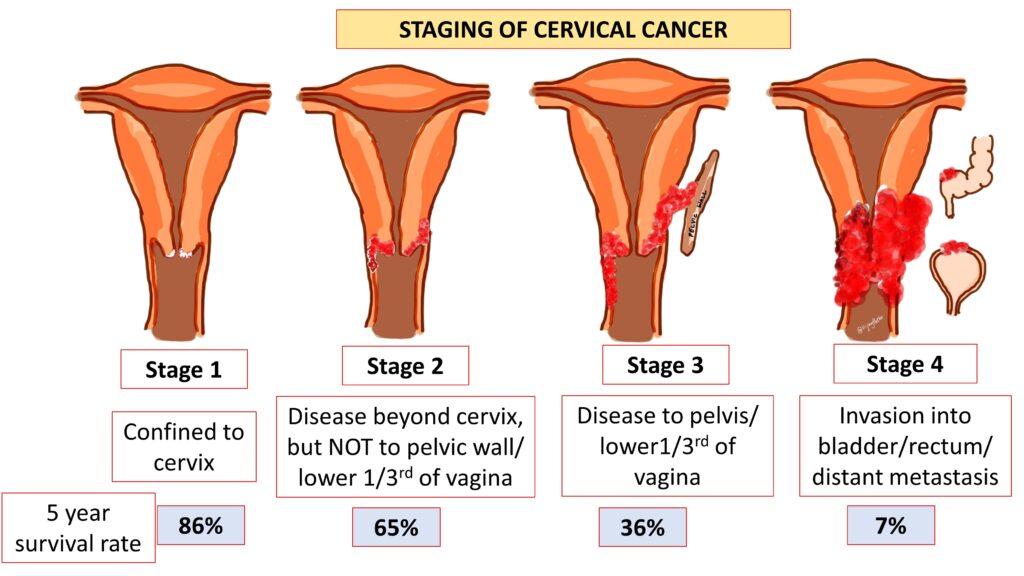
Clinical features
Majority of the patients presents with abnormal pap smear during screening programs.Average age- 45 – 50 yrs
However, Symptoms include
a. Postcoital or intermenstrual bleeding- Stage 1b or higher
b. Obstructive uropathy and renal failure – With growth into parametria and involvement of ureters,
c. Pain – pelvic wall or lumbosacral nerve root invasion.
d. hematuria, rectal bleeding, or constipation- bladder or rectal Involvement in advanced stages
Treatment
Superficially invasive squamous cell carcinomas- Cervical cone excision
Invasive cancers – Hysterectomy with lymph node dissection
Advanced lesions – Radiation and chemotherapy
Click on the link below to view the vido tutorial on cercical intraepithelial neoplasia and cervical cancer





Recent Comments