Gestational Trophoblastic Diseases: Part 1: Complete and Partial Hydatidiform Moles
What are gestational trophoblastic diseases?
Gestational trophoblastic diseases (GTDs) are a spectrum of tumors and tumor-like conditions characterized by the abnormal proliferation of placental tissue. This proliferation can involve the villous or trophoblastic components of the placenta.
GTDs are heterogeneous in presentation, both clinically and histopathologically, and are commonly associated with a history of pregnancy.
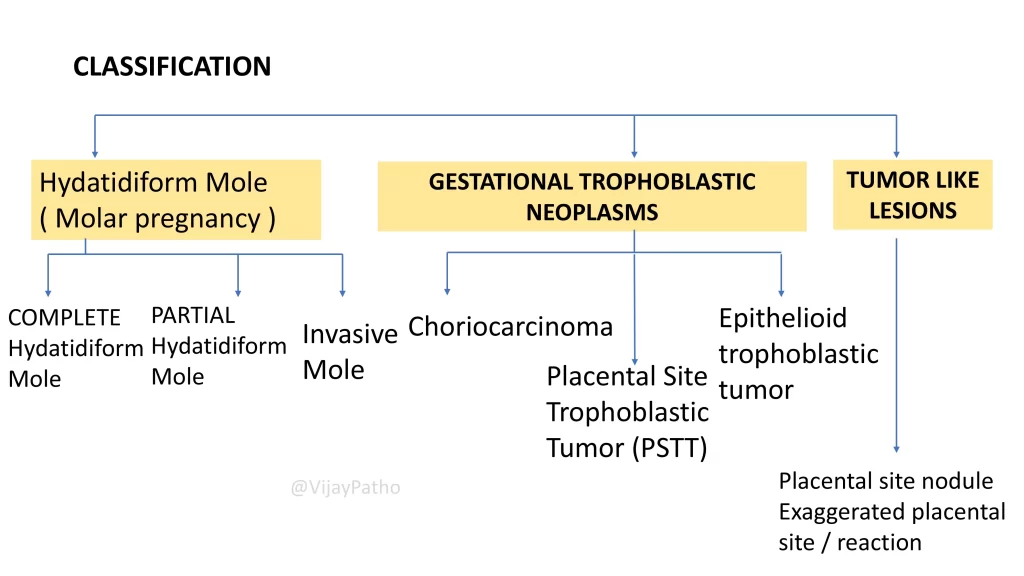
How are GTDs classified?
GTDs are broadly categorized into three types:
Molar Pregnancy (Hydatidiform Mole):
Complete Hydatidiform Mole
Partial Hydatidiform Mole
Invasive Mole
Gestational Trophoblastic Neoplasms:
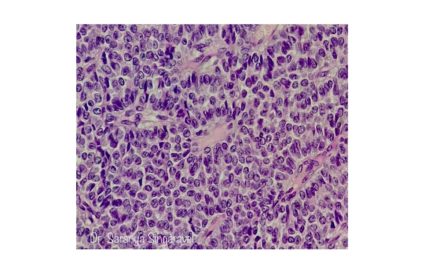
Choriocarcinoma
Placental Site Trophoblastic Tumor
Epithelioid Trophoblastic Tumor
Tumor-like Lesions:
Placental Site Nodule
Exaggerated Placental Site Reaction
What is a hydatidiform mole (molar pregnancy)?
Hydatis: A Greek word meaning “drop of water,” representing the watery appearance of the villi.
Forma: A Latin word meaning “shape or form.”
Mole: A Latin term referring to something heavy or large, analogous to the heavy uterus in molar pregnancies.
What are the common features of GTDs?
All GTDs involve abnormal growth of placental trophoblastic cells, including cytotrophoblasts, syncytiotrophoblasts, or intermediate trophoblasts.
What is the basic structure of the placenta?
The placenta is a temporary, disk-shaped organ formed from embryonic tissues of the fetus. Its key functional unit is the chorionic villus, finger-like projections responsible for maternal-fetal exchange. These villi are lined by:
Cytotrophoblasts: Inner proliferative layer.
Syncytiotrophoblasts: Outer sheet-like layer secreting hCG and aiding implantation.
Intermediate trophoblasts are also present and play a role in trophoblastic disorders.
What are the risk factors for molar pregnancies?
Risk factors include:
Maternal age below 20 or above 35 years.
Low dietary intake of carotene.
AB blood group.
History of prior molar pregnancies.
How common are molar pregnancies?
In the United States: 1 in 1,000 to 2,000 pregnancies.
In Southeast Asia: 1 in 500 to 1,000 pregnancies.
What is the pathogenesis of complete and partial hydatidiform moles?
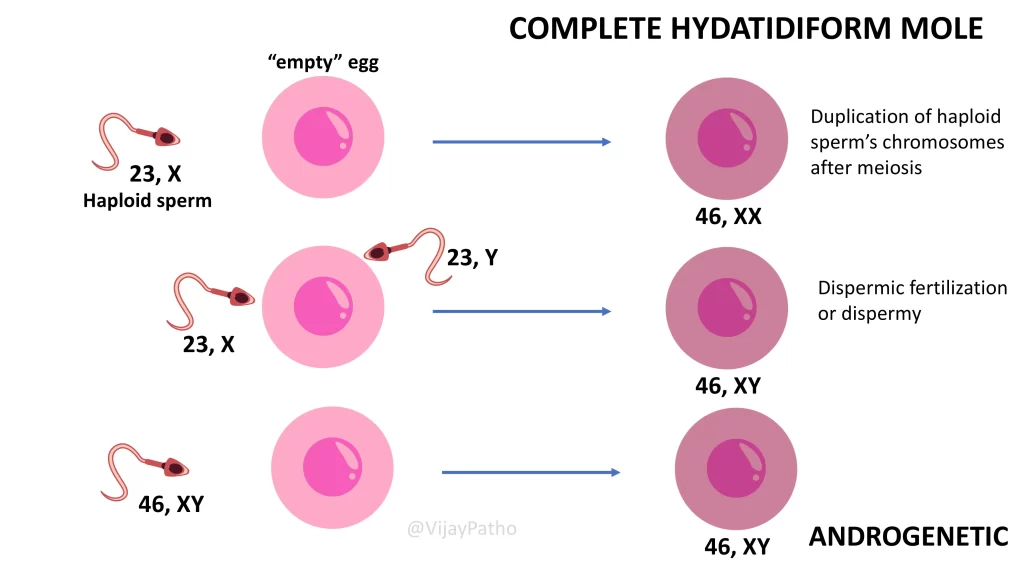
Complete Mole: Results from fertilization of an egg that has lost its female chromosomes (“empty egg”) by a single sperm, which duplicates its chromosomes, or by two sperms. The resulting karyotype is diploid (46XX or 46XY) and entirely paternally derived.
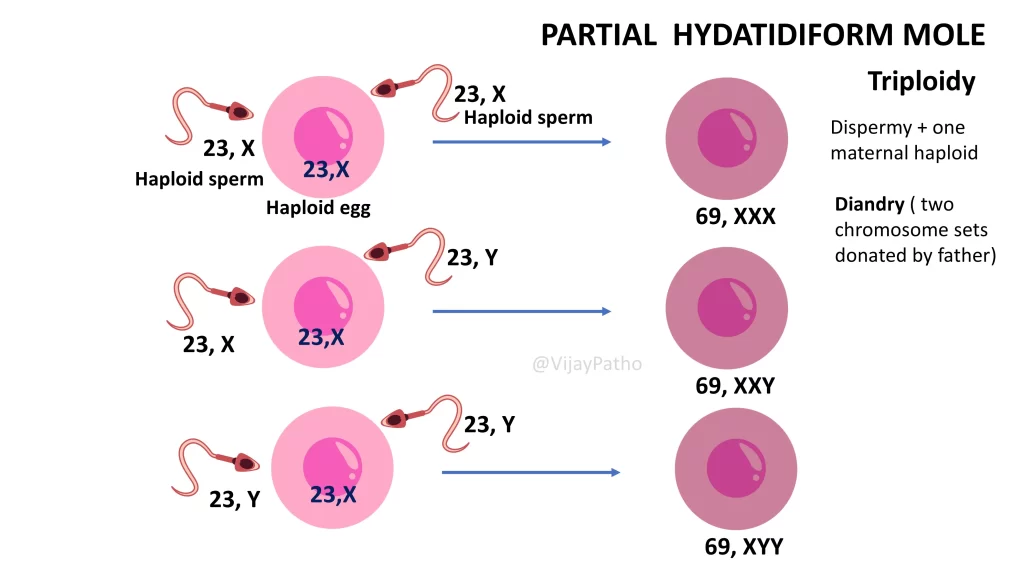
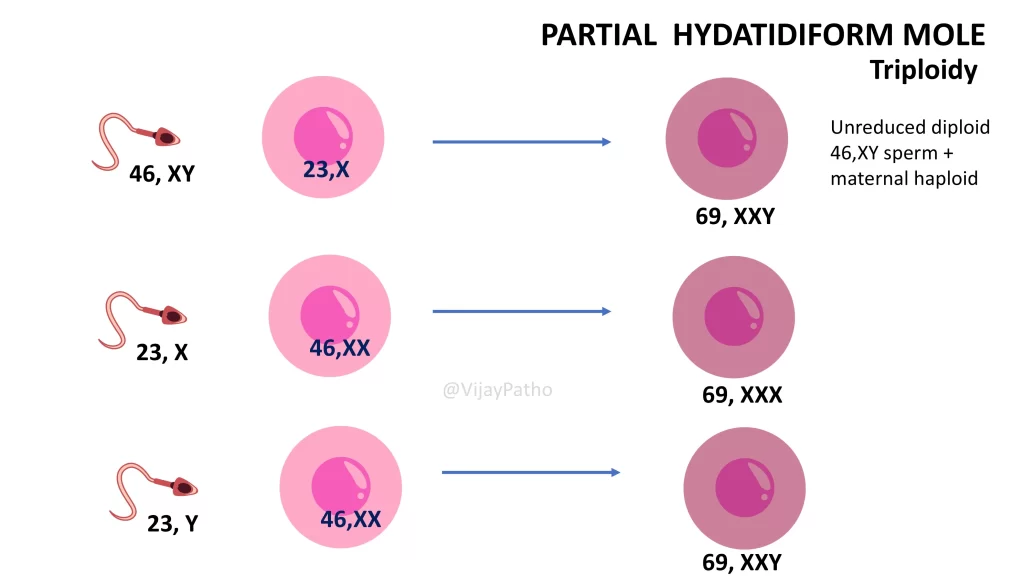
Partial Mole: Arises from fertilization of a normal egg by two sperm, leading to a triploid karyotype (69XXX, 69XXY, or 69XYY). It contains both maternal and paternal chromosomes.
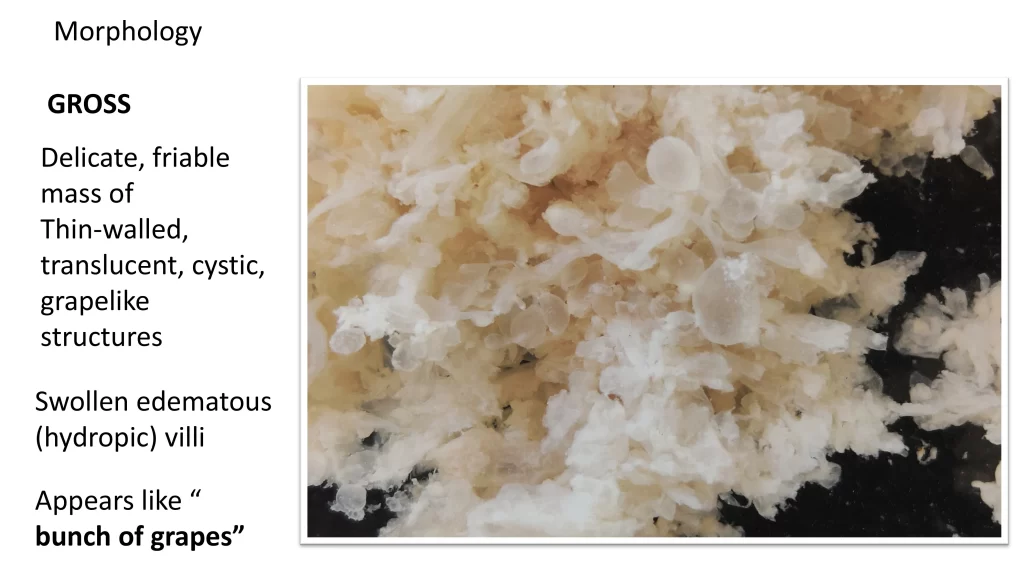
What are the gross morphological features of a hydatidiform mole?
Delicate, friable mass with thin-walled translucent cystic structures resembling a bunch of grapes.
What are the morphological differences between complete and partial moles?
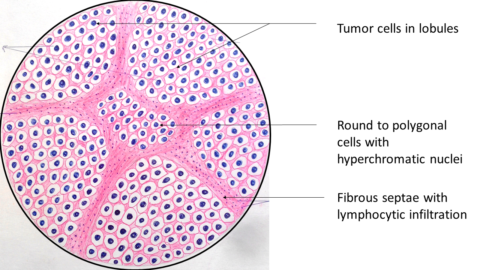
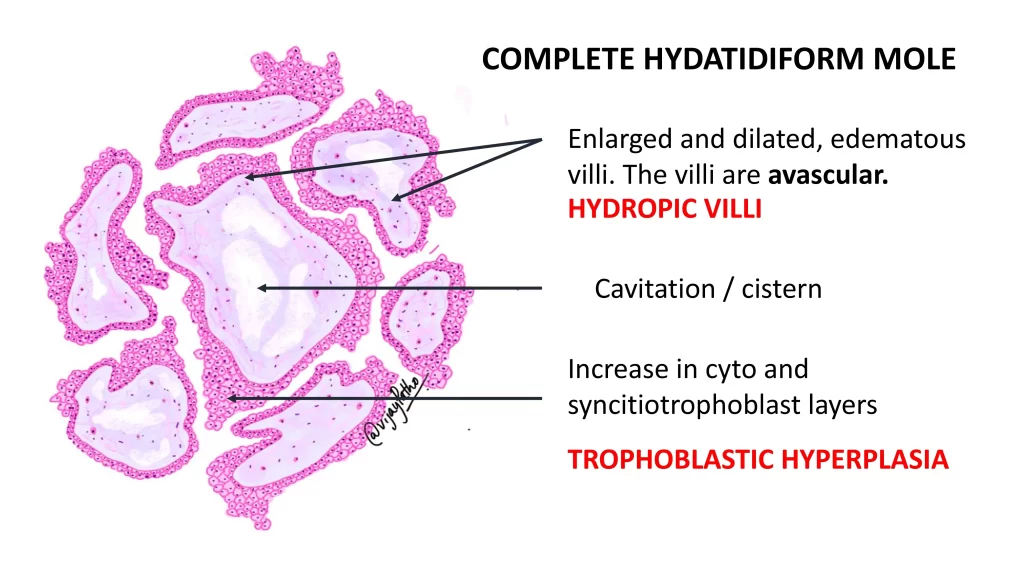
Complete Mole:
All or most villi are swollen and edematous (hydropic).
Absence of fetal development and vasculature.
Diffuse trophoblastic hyperplasia (cytotrophoblast and syncytiotrophoblast).
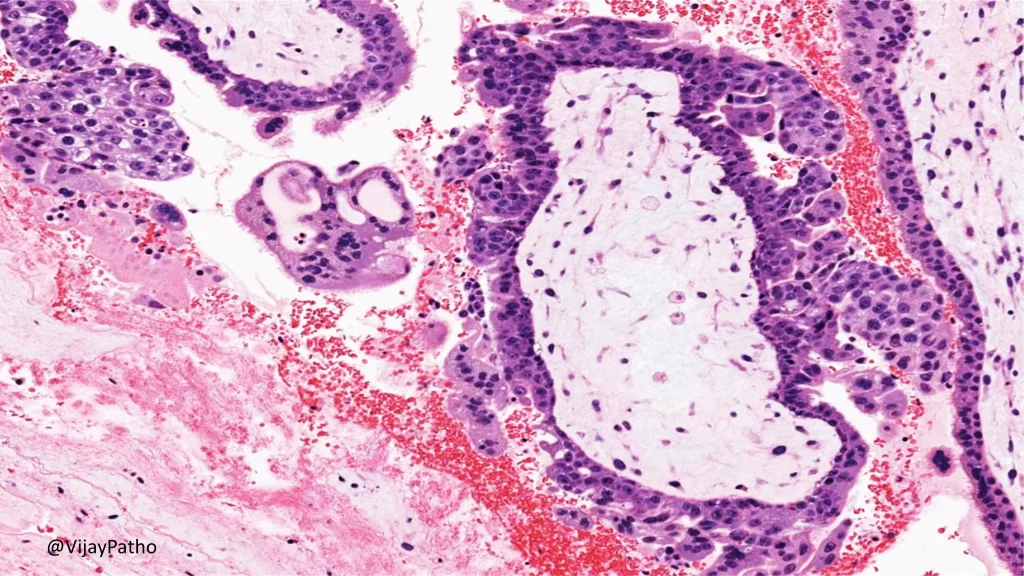
Partial Mole:
Only some villi are hydropic.
Presence of fetal tissue or embryo.
Focal trophoblastic hyperplasia.
How do molar pregnancies present clinically?
Common symptoms include:
Vaginal bleeding (most common).
Hyperemesis (severe nausea and vomiting).
Passage of grape-like vesicles.
Abdominal pain (rare).
What is the diagnostic approach for molar pregnancies?
Clinical Suspicion: Exaggerated pregnancy symptoms such as hyperemesis.
Serum beta-hCG Levels: Typically >100,000 IU/L.
Ultrasound: Classic “snowstorm appearance.”
Histopathology: Definitive diagnosis with characteristic findings.
How can complete and partial moles be differentiated histologically?
Complete Mole: Enlarged, avascular villi with diffuse trophoblastic hyperplasia.
Partial Mole: Enlarged villi with focal trophoblastic hyperplasia and presence of fetal blood vessels.
What is the role of P57 immunostaining in differentiation?
Complete Mole: Negative for P57.
Partial Mole: Positive for P57.
How are molar pregnancies treated?
Suction Curettage: Most common treatment.
Hysterectomy: Advised for women over 35 or those who have completed their families to reduce the risk of GTNs.
Follow-Up: Monitoring beta-hCG levels for 6 months to 1 year to ensure they return to non-pregnant levels.
What are the complications and prognosis of molar pregnancies?
Complete Mole:
2.5% risk of choriocarcinoma.
15% risk of persistent or invasive mole.
Partial Mole:
Risk of persistent molar disease.
Not associated with choriocarcinoma.
Why is differentiation between complete and partial mole important?
Clinicians need to identify the type of mole to assess the risk of progression to GTNs, particularly choriocarcinoma, which is associated only with complete moles.