Define Anemia
Anemia is defined as a reduction of total circulating red cell mass or hemoglobin concentration or oxygen carrying capacity of blood below normal limits that is expected for a healthy person of same age and sex in the same environment.
You can measure anemia by either reduction in hematocrit or by the hemoglobin concentration
We can divide them based on morphology or etiology.
Etiological classification could be due to impaired production or increased destruction or due to blood loss
Impaired red cell production mainly occurs in deficiency anemia which is nutritional.
In India, the two most common cause of deficiency anemias include iron deficiency and Vitamin B12 deficiency (megaloblastic anemias).
IRON DEFICIENCY ANEMIA (IDA)
It is the most common cause of anemia worldwide. Erythropoiesis as we know requires iron. Iron deficiency anemia develops when body iron stores are depleted, level of circulating iron reduced, and there is insufficient iron available for erythropoiesis.
Iron requirements:
Iron is mainly supplemented through diet.Dietary sources of iron are meats, eggs and green leafy vegetables.
Daily requirements are as given below and it varies according to age and sex. Normal daily western diet contains 10-20 mg of iron and about 10% gets absorbed through intake which balances loss of 1 mg daily.
Up to 4 months :0.5 mg
children :1 mg
Menstruating women :3 mg
Pregnancy: 3-4 mg
Adult men and postmenopausal women: 1 mg
Females need higher dietary requirements of iron due to menstrual blood loss and increased demand especially during pregnancy. Hence, iron deficiency is frequently seen in females. Elderly individuals especially men, rarely present with iron deficiency anemia. Chronic blood loss due to malignancy in the gastrointestinal tract could be one of the very important reason of IDA that cannot be neglected.
How and where is iron absorbed?
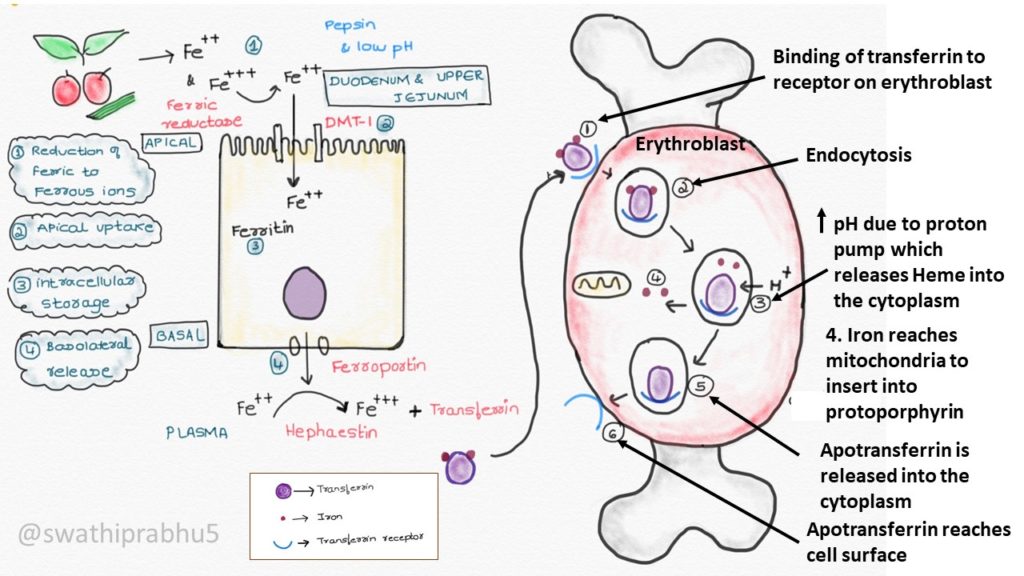
Iron is released in Fe +2 or Fe+3 from complex found in food substance. Absorption occurs only in the form of Fe+2. So all the Fe+3 are converted to Fe+2 by Ferric reductase which is present in the apical region of the intestinal epithelial cells, aided by pepsin and low pH of stomach. Absorption occurs in the duodenum and upper jejunum. Fe+2 enters intestinal epithelial cells with the help of DMT-1(Divalent metal transporter-1).
Iron can be stored inside the epithelial cells of intestine as ferritin. It enters plasma by ferroportin. After this it has to be transported to erythrocytes in the marrow for erythropoiesis which occurs with the help of transferrin. But transferrin binds only to Fe+2 for of iron. Hence Fe+3 converted to Fe+2 by Hephaestin which is present in the basal layer of the epithelial cells. Transferrin can bind to two atoms of iron. Transferrin carries it to erythroblasts which has transferrin receptor on its surface. Once transferrin binds to the receptor , iron is internalized by endocytosis. Rest of the process is shown in the image below
What are the causes of Iron deficiency anemia?
1) Inadequate intake: eat healthy and balanced diet to keep all deficiencies at bay
2) Defective absorption: Gastrointestinal diseases like celiac disease, gastrectomy
3) Loss of iron: Bleeding, malignancy, Crohn’s disease
4) Increased requirements: Pregnancy, infancy, adolescents
What are the clinical features of iron deficiency anemia?
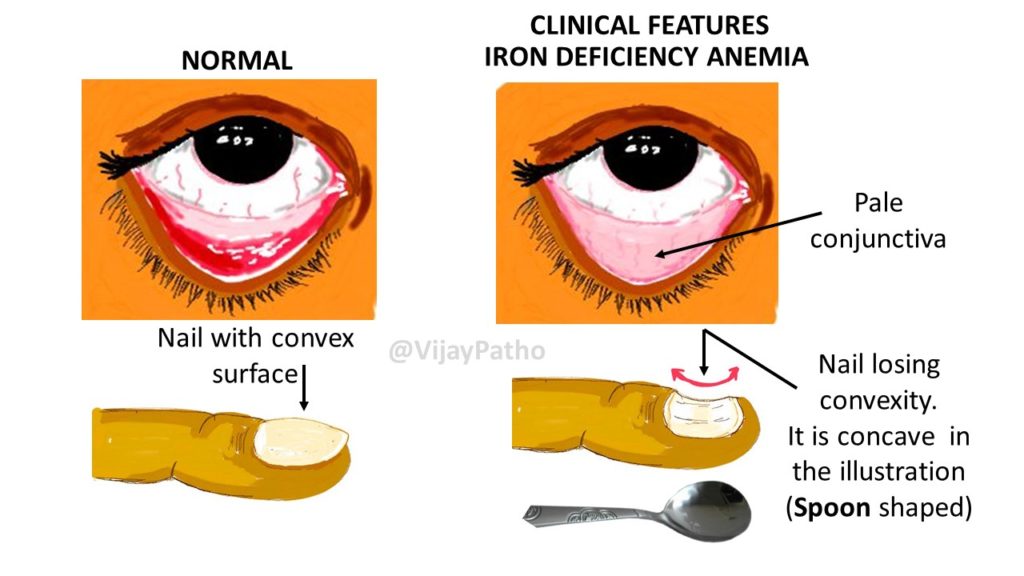
We usually encounter this clinical scenario during our clinical postings. Look out for weakness, easy fatiguability, breathlessness, tachycardia, systolic heart murmur. Pallor is one of the most important sign.
Pica: abnormal and intense desire to eat strange substances such as mud, clay, hair etc
Koilonychia: spoon shaped nails
Atrophic glossitis, angular stomatitis can also be seen
What is Plummer-Vinson syndrome?
Triad of Iron deficiency anemia, dysphagia and glossitis is known as Plummer-Vinson syndrome (or Patterson-Kelly syndrome)
Mention stages of Iron deficiency Anemia
There are three stages
1) Depletion of storage iron
All the parameters are normal except for S.ferritin and bone marrow iron which is absent/ reduced.
Can be remembered as when you are out of money you first fill your purse (transferrin) with money from ATM (storage iron)
2) Iron-deficient erythropoiesis:
Iron is used up from the transferrin. TIBC is normal of increased, Transferrin saturation is decreased. However, MCV is still normal
3) Iron deficiency anemia:
Full blown picture of IDA as described above with decreased MCV
Now let’s focus on the laboratory investigations of Iron deficiency anemia.
A person with pallor walks in to your clinic. How do you proceed.
Clinical examination a first step
1) Order Complete blood count
Hemoglobin and hematocrit is reduced
Red cell indices: Reduction in MCV, MCH and MCHC and increase in Red cell distribution width.
2) Peripheral blood examination:
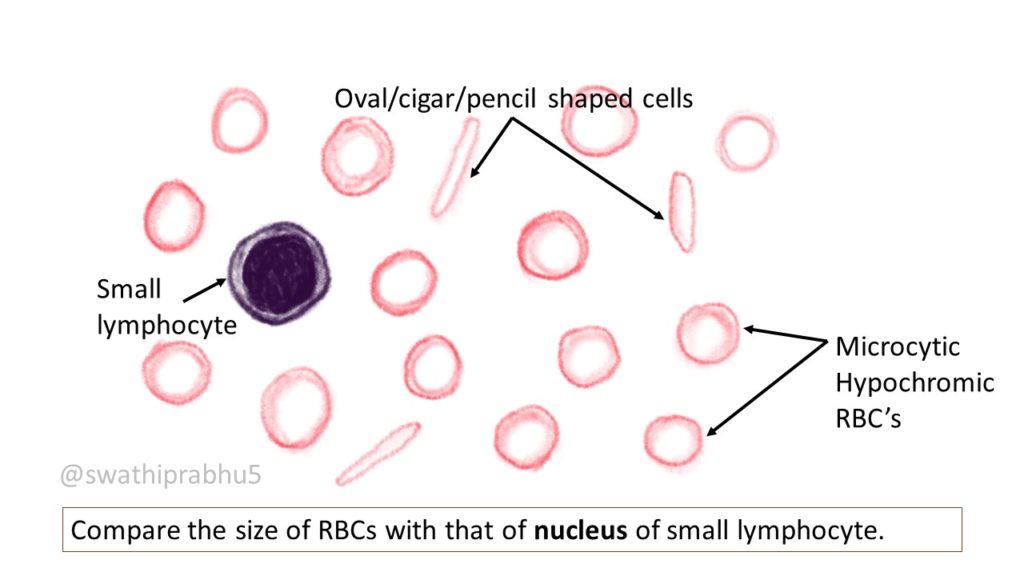
Microcytic hypochromic cells indicate towards iron deficiency. However, microcytes can also be seen thalassaemia minor or long-standing anemia of chronic disease (usually normocytic normochromic).
You can also see elongated cells, pencil shaped cells, elliptocytes.
Now you order for biochemistry investigations to confirm iron deficiency anemia. They include
a) Serum iron: depleted (normal 50- 150 mg/dl)
b) Serum TIBC (total iron binding capacity): increased (normal 300-400 mg/dl)
c) Transferrin saturation: reduced (normal is 20-55%)
d) Serum ferritin: reduced (normal 15-300 mg/L)
Some recent and new modalities include
Serum Transferrin Receptor assay(TfR) assay: increased
Free erythrocyte protoporphyrin (FEP): increased
Bone marrow examination: it is usually not done in iron deficiency anemia. What we see are called micronormoblasts in the marrow. They are normoblasts which have become smaller in size. They have reduced amount of cytoplasm that is vacuolated and has ragged cell borders. Hemoglobinisation of cytoplasm is defective
What are other conditions you can see microcytes in the blood smear?
Thalassemia minor, long standing cases of anemia of chronic disease and sideroblastic anemia
How do you treat iron deficiency anemia?
Mild cases can be treated by oral iron therapy.
Severe cases can be treated by parenteral therapy. We have injectable forms which are usually given as intramuscular injections. Blood transfusions can also be done in severe cases.