What is seminoma?
Seminoma is a germ cell tumor and one of the most common types of testicular tumors, comprising about 50% of germ cell tumors. It primarily affects males in the fourth decade of life . Seminomas have an excellent prognosis due to their high radiosensitivity and chemosensitivity.
What factors contribute to the pathogenesis of germ cell tumors?
Germ cell tumors arise due to:
Environmental Factors:
Exposure to pesticides and non-steroidal estrogens in utero can lead to testicular dysgenesis syndrome (cryptorchidism, hypospadias, and poor sperm quality). Cryptorchidism is associated with approximately 10% of testicular germ cell tumors including seminomas.
Genetic Factors:
Mutations in genes like KIT (linked to familial germ cell tumor risk) and BAX (involved in apoptosis) are significant.
Germ cell tumors are 4x more common in fathers/sons and 8-10x higher in brothers of affected individuals.
For more details of classification : Classification of testicular tumors
Discuss the pathogenesis of germ cell tumors?
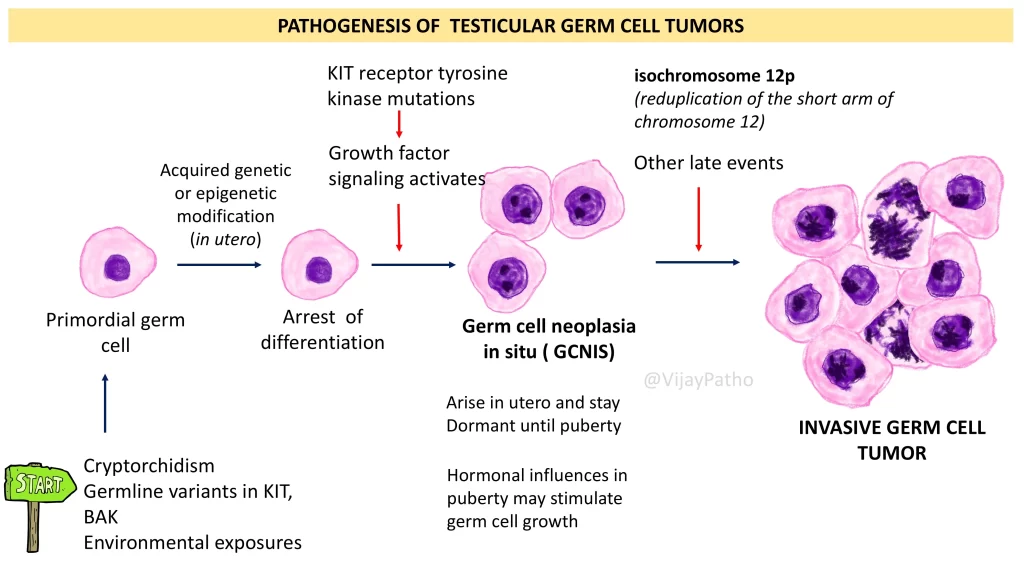
The process involves: ( See the illustration below)
Arrest of differentiation in primordial germ cells due to genetic, epigenetic, or environmental factors.
Formation of germ cell neoplasia in situ (GCNIS), a precancerous condition that arises in utero but remains dormant until puberty.
Activation during puberty due to hormonal influences or chromosomal alterations, such as duplication of the short arm of chromosome 12, leading to invasive germ cell tumors.
What are the clinical features of seminoma?
Seminomas typically present as a painless swelling in the groin, with possible mild pain or discomfort in the testes, groin, or lower abdomen. In some cases, patients may seek supportive treatments such as nerve pain relief options to manage discomfort associated with pressure or inflammation in surrounding tissues.
Advanced cases may cause symptoms due to metastasis, such as lower back pain.
Rarely, seminomas are associated with paraneoplastic syndromes like polycythemia, exophthalmos, autoimmune hemolytic anemia, or membranous glomerulonephritis.
How do seminomas metastasize?
Via lymphatics to retroperitoneal, mediastinal, or cervical lymph nodes, particularly the left supraclavicular group.
Rarely, seminomas metastasize hematogenously to other organs.
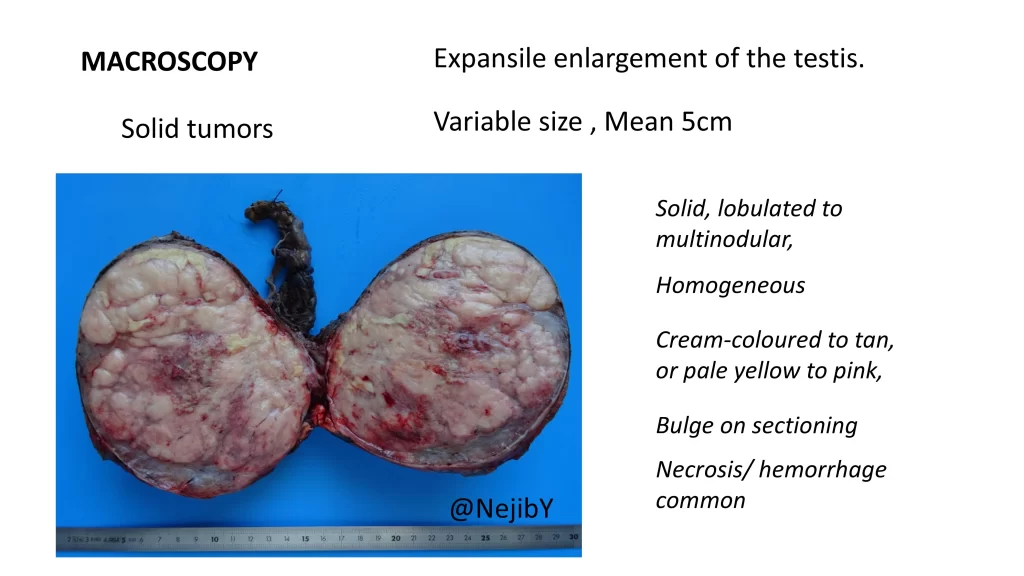
What are the macroscopic features of seminoma?
Seminomas are solid, lobulated tumors with a homogeneous cream-to-tan cut surface.
Larger tumors may show areas of necrosis and hemorrhage.
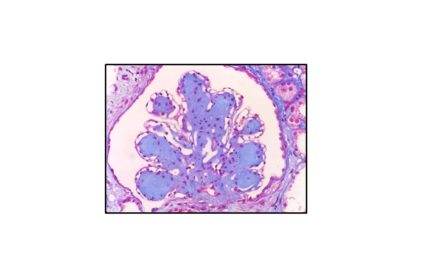
What are the microscopic features of seminoma?
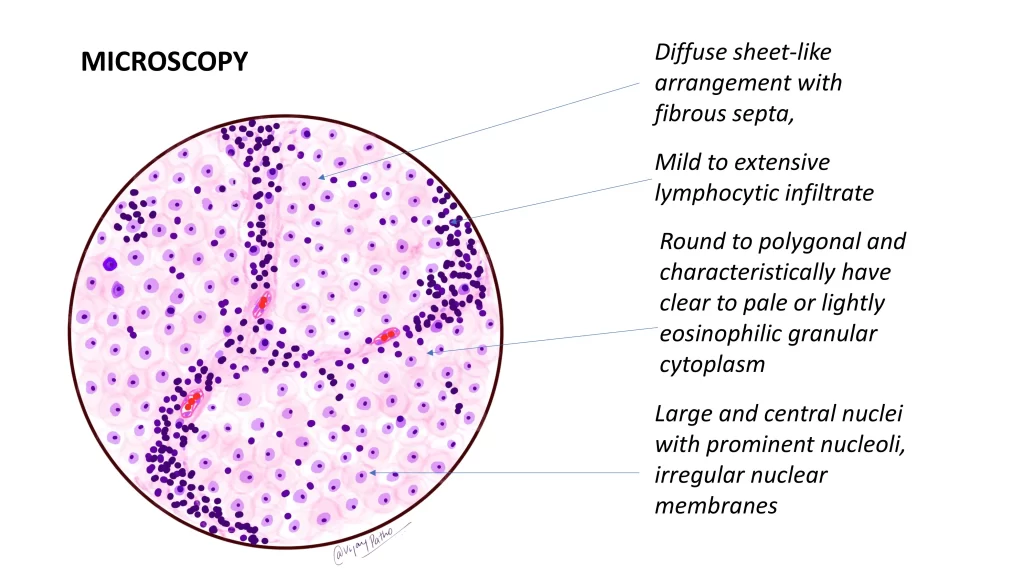
Tumor cells are arranged in sheets separated by fibrous septa infiltrated with lymphoplasmacytic cells.
Cells are large, round to polygonal, with clear or pale cytoplasm, centrally placed nuclei, and prominent nucleoli.
Ill-formed granulomas may be seen.
What are the immunohistochemical markers for seminoma?
Positive for KIT (CD117), OCT3/4, PLAP, and podoplanin.
Negative for cytokeratin.
How are seminomas staged clinically?
Stage I: Confined to the testis.
Stage II: Spread to retroperitoneal or pelvic lymph nodes.
Stage III: Metastasis above the diaphragm or to distant organs.
What is the treatment and prognosis of seminoma?
Stage I and II: Managed with orchiectomy, with or without chemotherapy/radiotherapy. Cure rates are approximately 95%.
Stage III: Treated with platinum-based chemotherapy, with better survival rates than other germ cell tumors.
Seminomas have the best prognosis among germ cell tumors.
Are there any serum markers for seminoma?
Serum HCG levels may be elevated, usually less than 1,000 mIU/mL, depending on the proportion of syncytiotrophoblastic cells in the tumor.
Click below to watch the video tutorial on seminoma