Introduction:
● GBM is the most common malignant primary brain cancer (WHO Grade IV)
● Essentially incurable, overall survival time from 12 to 18 months, less than 5% of patients survive longer than five years after diagnosis
Previously named as “glioblastoma multiforme” due to cut section being variegated (yellowish necrotic central area, grayish peripheral rim, recent and old hemorrhage, cysts due to liquefied necrotic tumor tissue) and having diverse histological features
● Mostly located in the supratentorial region with the highest incidence in the frontal lobe, multiple lobes (overlapping tumors), followed by the temporal and parietal lobes
Pathogenesis:
● Cellular origin of glioblastoma is unknown
● Assumed to originate from glial-type cells due to similarities in immunostaining of glial cells and glioblastoma
● Tumor can contain neoplastic astrocytes that are poorly differentiated
● The tumor can result in a diffuse infiltrative growth pattern
● Glioblastomas originate in the cerebral white matter, grow quickly, and can become very large before producing symptoms
● The tumor could extend into the meninges or ventricular wall, generating high protein content in the CSF, as well as lymphocytic pleocytosis
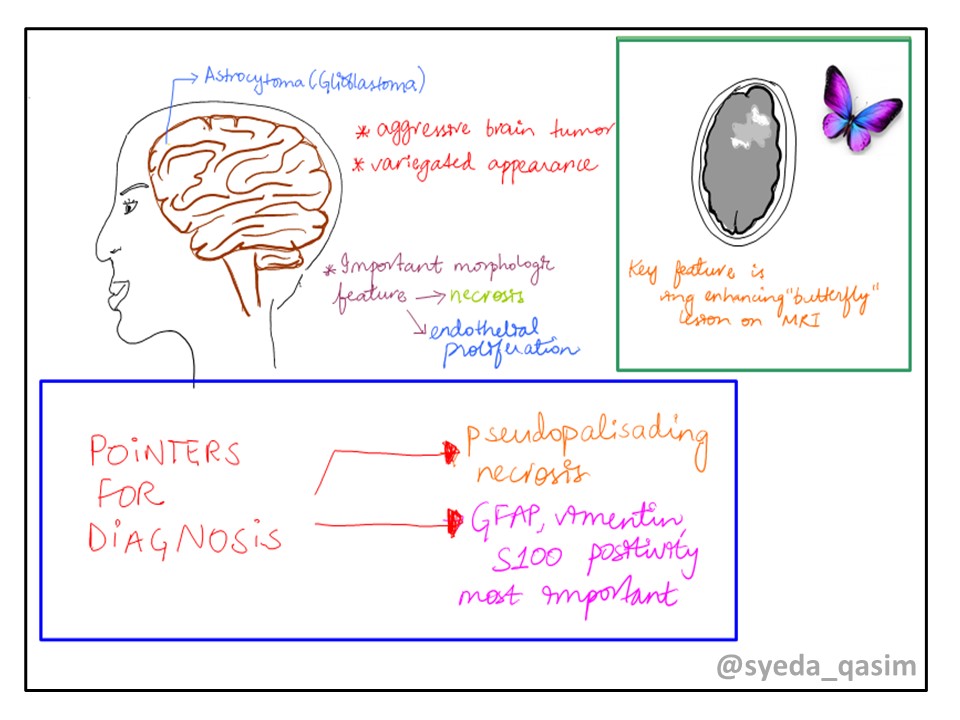
Figure 1: Typical features of Glioblastoma
Demographics and Risk Factors:
● Slightly more common in men
● Risk Factors include: ionizing radiation
● Exposures to synthetic rubber, vinyl chloride or pesticides
● Genetic disorders such as Turcot syndrome, Li-Fraumeni syndrome, Lynch syndrome, Neurofibromatosis type 1, Cowden syndrome
Glioblastoma classification:
● Brain tumor classification has been traditionally based on histopathology at macroscopic level, measured in hematoxylin-eosin sections
Glioblastomas are mainly classified according to the status of isocitrate dehydrogenase (IDH) mutation: IDH-wildtype or IDH-mutant
● Four subtypes of glioblastoma have been identified based on gene expression:
1. Classical: Around 97% of tumors in the classical subtype contain additional copies of the epidermal growth factor receptor (EGFR) gene, and most have higher than normal expression of EGFR. The TP53 (p53) gene, which is often mutated in glioblastoma, is rarely mutated in this subtype
2. Proneural: has high rates of alterations in TP53 (p53), and in PDGFRA, the gene encoding a-type platelet-derived growth factor receptor, and in IDH1, the gene encoding isocitrate dehydrogenase-1
3. Mesenchymal: has alterations in NF1 gene (neurofibromin 1) and lesser of the characteristic alterations in the EGFR gene
4. Neural: has the expression of neuron markers such as NEFL, GABRA1 and SYT1
● The genetic alterations in glioblastoma are described on the basis of two pathways, the RB and the PI3K/AKT
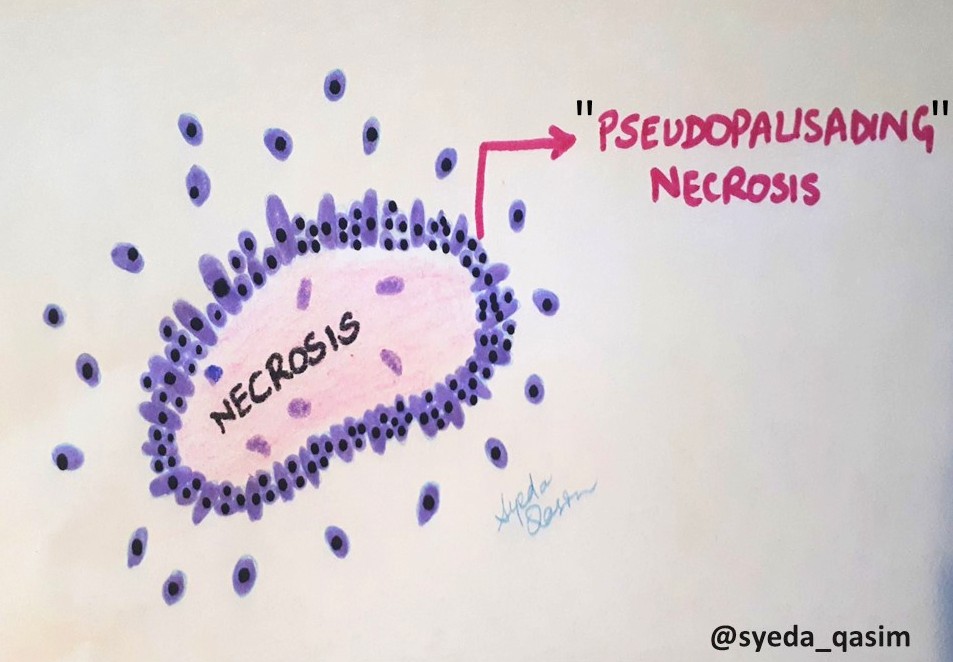
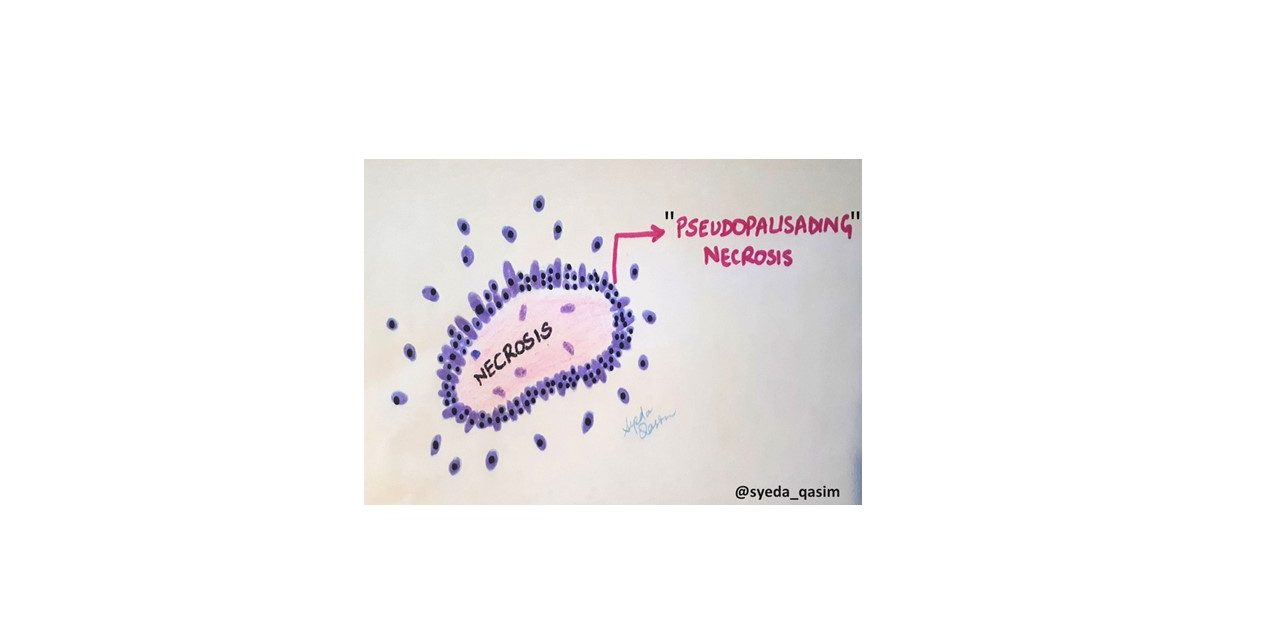
Figure 2: Characteristic pseudopalisading necrosis in Glioblastoma
Diagnosis:
● The “classical” not to miss sign for glioblastomas on MRI is ring-enhancing lesions (has a broad list of differentials, discussed below)
● The gold standard for diagnosis is pathology.
● On gross appearance, there may be presence of a pseudocapsule in rapidly growing tumors
● Mostly solitary but can cross midline through corpus callosum to produce a “butterfly” lesion
● Large tumors are poorly delineated with accompanying peritumoral edema
● Two morphologic features critical for diagnosis are necrosis and endothelial proliferation (microvascular proliferation) showing thickened vascular walls due to endothelial cell hyperplasia and hypertrophy
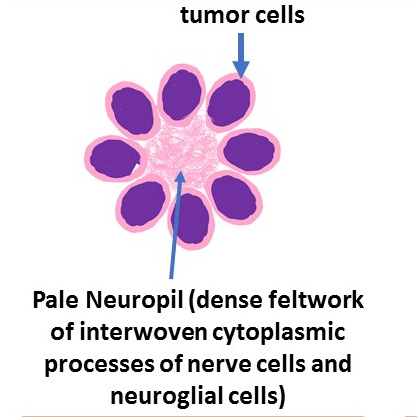
● The tumor shows serpiginous necrosis with palisading around necrotic foci (pseudopalisading necrosis)
● Small cell morphology: densely packed small cells, resembles anaplastic oligodendroglioma on low power, may be calcification, perivascular pseudorosettes
● The most important positive stains are GFAP, vimentin, S100, AE1 / AE3 ( > 95%)
● Key negative stains are IDH R132H and ATRX
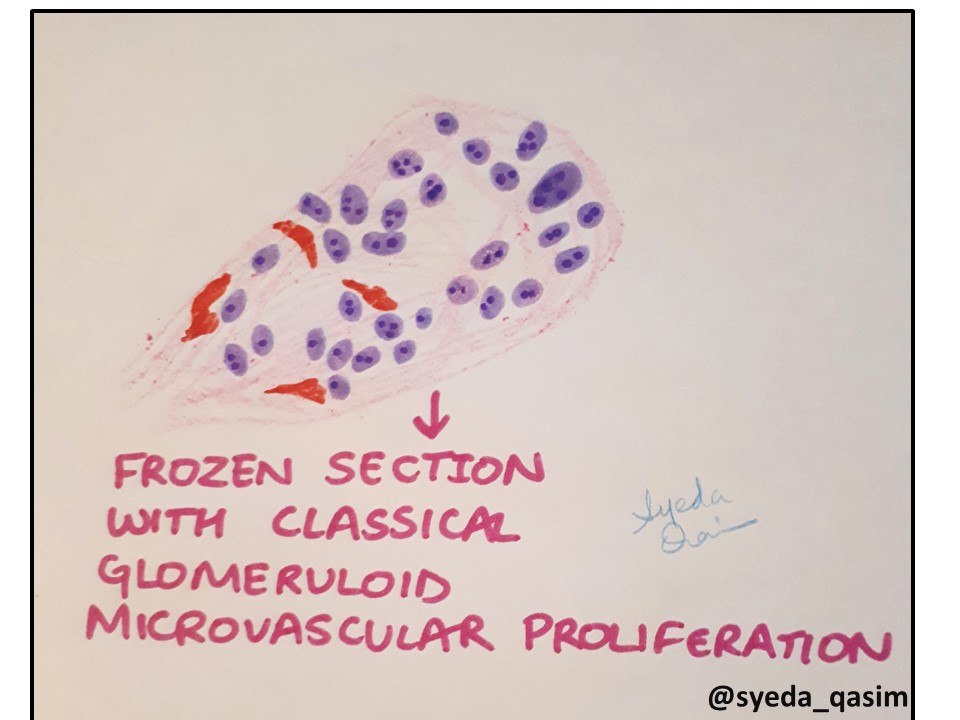
Figure 3: Microvascular proliferation in glioblastoma
Clinical Presentation:
● Symptoms of a classical space occupying lesion (SOL): headache, nausea and vomiting, change in headache pattern, abnormal neurologic exam, worsening headache with changes in body position (e.g., bending over) and Valsalva maneuvers, seizures, cognitive change with a possible focal neurologic deficit
Most Important Points to Remember:
● WHO grade IV glial neoplasm, one of the highly aggressive malignancies causing death in most patients in <1 year
● The most polymorphic of any known neoplasm, a reason for its previous characterization “Glioblastoma multiforme” suggesting multiple forms
● Two morphologic features essential for diagnosis: necrosis and endothelial proliferation
● The tumor shows serpiginous necrosis with palisading around necrotic foci
● Key differential diagnosis are meningioma (EMA positivity, containing entrapped GFAP+ glia), lymphoma (CD45 positivity with angiocentric and angioinvasive patterns) and other high grade gliomas



Recent Comments