ENDOMETRIAL CARCINOMA
Endometrial carcinoma
Most common invasive cancer of the female genital tract
Accounts for 7% of all invasive cancer in women
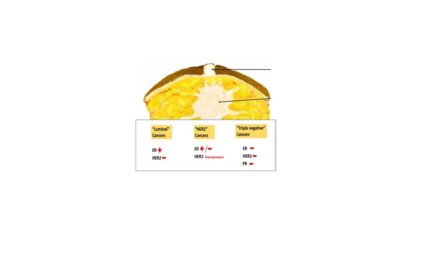
Classification:
Type I- endometrioid type – they mimic proliferative endemetrial glands
Type II- Serous type
Endometrioid endometrial carcinoma
Risk factors
Unopposed estrogenic stimulation of endometrium
Obesity
Hypertension
Diabetes mellitus
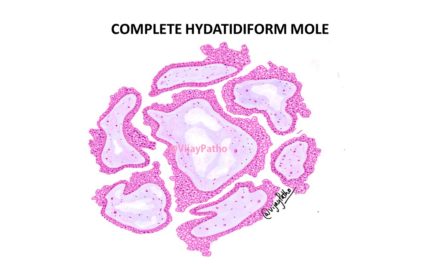
Precursor lesion – Endometrial hyperplasia
Pathogenesis
Hallmark of endometrioid endometrial carcinoma – Increased signaling through the PI3K/AKT pathway by various mutations which leads to increase in expression of ER –dependent target genes in endometrial cells.
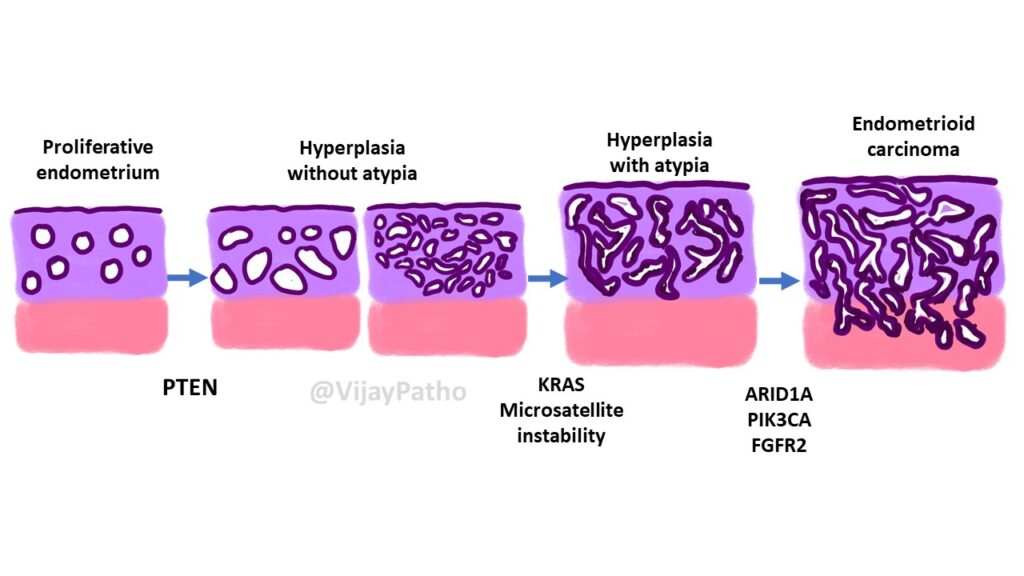
The mutations involved are
PTEN tumor suppressor gene
PIK3CA mutations
KRAS
ARID1A
POLE gene mutations
TP53 gene mutations
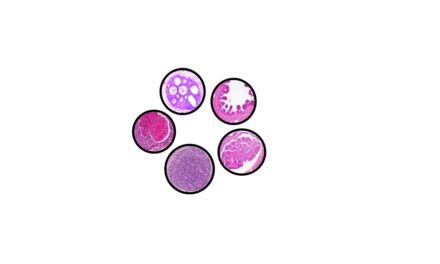
The progression of various lesions resulting in endometrial carcinoma is as illustrated below.
Morphology
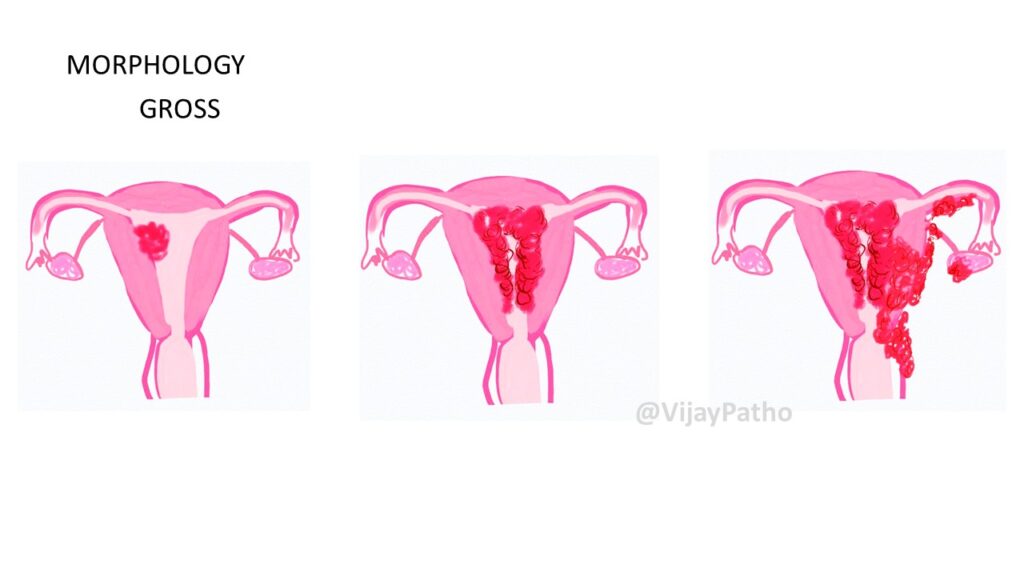
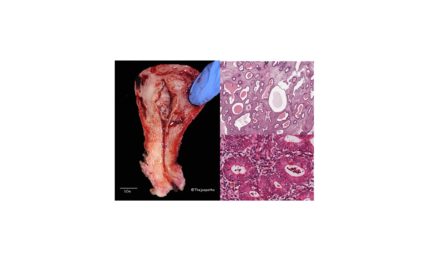
Gross: The lesions can be localized polypoidal lesion to diffusely infiltrative and may extend into and outside the pelvis as illustrated below
Microscopy:
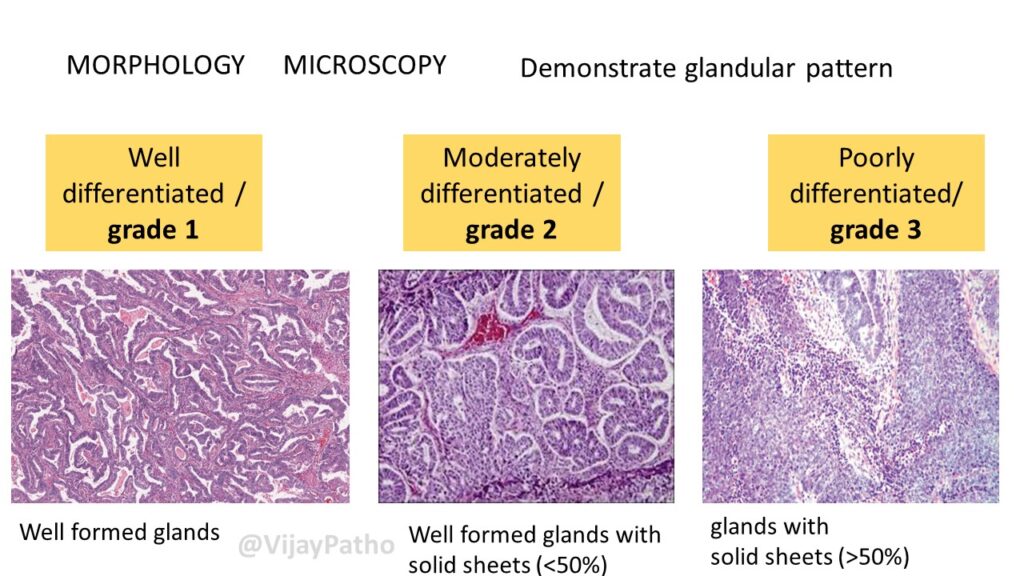
Demonstrate glandular pattern and are classified into
1. Well differentiated / grade 1 – Well formed glands
2. Moderately differentiated / grade 2 – Well formed glands with solid sheets (<50%)
3. Poorly differentiated/ grade 3 – glands with
solid sheets (>50%)
Serous endometrial carcinoma
NOT ASSOCIATED WITH ESTROGEN STIMULATION
Type II tumors, 15% of endometrial cancers
10 years older than those with endometrioid type
Occur in the setting of endometrial atrophy
Precursor lesion– Serous endometrial intraepithelial carcinoma
Morphologic and biologic overlap with ovarian serous carcinoma.
Pathogenesis : highly associated with disruptive mutations in the TP53 tumor suppressor gene
Morphology: GROSS – Arise in small atrophic uteri. large bulky tumors or deeply invasive into the myometrium.
MICROSCOPY – Papillary growth pattern composed of cells with marked cytologic atypia
CLINICAL FEATURES
Uncommon in women < 40 years
40-65 years – peak incidence.
Initially asymptomatic, Later irregular or post menopausal bleeding
Diagnosis – Histologic examination of D&C specimen
During diagnosis, DNA Analysis for mismatch repair defects done because 3-5% have Lynch Syndrome, and are at high risk for colon carcinoma.
TREATMENT
ENDOMETRIOID carcinoma- Surgery with adjuvant radiation. Chemotherapy if the spread is beyond uterus
SEROUS carcinoma – Chemotherapy irrespective of spread
Inhibitors of the PI3K/AKT pathway are being tried
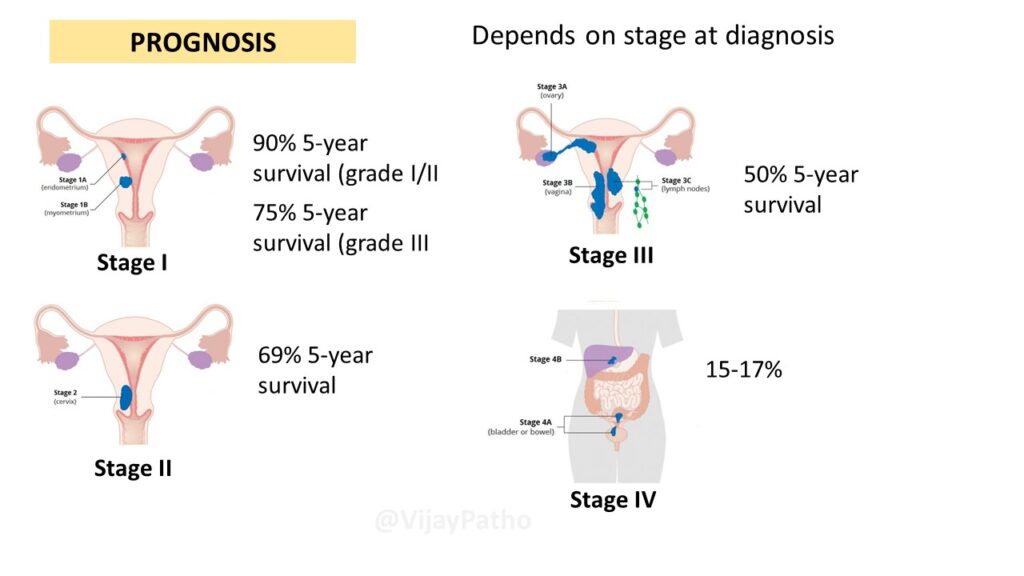
Prognosis: Depends on stage at diagnosis
Stage I: tumor confined to uterus. 90% 5-year survival (grade I/II). 75% 5-year survival (grade III
Stage II: Tumor extending into cervix. 69% 5-year survival
Stage III- Tumor extending into the adnexa and lymphnodes but not to adjacent bladder or rectum. 50% 5-year survival
Stage IV- Tumor spread to bladder/ rectum or metastasis to distant organs. 15-17% survival.
Click here to view the tutorial online. https://www.youtube.com/watch?v=Kb5_ZJjwgpg




Recent Comments