Define Inflammation
Inflammation is defined as a local response of living tissue to any injurious agent. This is basically a protective response needed for survival.
Historical aspects:
The word inflammation from the Latin inflammare (to set on fire).
Celsus , Roman Writer 1st century AD listed the four signs of inflammation.
He mentioned “rubor et tumor cum calore et dolore” which meant “redness and swelling with heat and pain”
The 5th Sign “Functio leasa” Loss of function Was added by Rudolf Virchow In 19th Century
John Hunter, Scottish surgeon:1793: inflammation is not a disease but just a response!
Elie Metchinkoff: 1880s; A Russian zoologist, Discovered the process of Phagocytosis
What are the types of inflammation and mention the differences
There are two types of inflammation. Acute and Chronic.
The differences are as below
Mention the steps of inflammatory response
The 5 “R”sSteps of inflammatory response
RECOGNITION of the injurious agent
RECRUITMENT of inflammatory cells ( leukocytes)
REMOVAL of the injurious agent
REGULATION ( control) of the inflammatory response
RESOLUTION/REPAIR
Mention the changes which occur in acute inflammation?
Vascular Changes
There will be increase in the blood flow
To bring cells and proteins to the site of injury
By vasodilatation & increased vascular permeability
Cellular events
Recruitment of leukocytes
Activation of leukocytes leading to the process of destruction of invaders and production of mediators.
By Phagocytosis
Want are the stimuli/triggers for acute inflammation
The stimuli/triggers are as below
Infections
Tissue necrosis
Trauma, physical and chemical agents
Foreign bodies
Immune reacions
How these stimuli are recognized by the host?
The antigen presenting cells/epithelial cells have RECEPTORS that sense these stimuli
These receptors are Toll like receptors and inflammasomes
Toll like receptors
- Microbial sensors
Present in plasma membrane & endosomes.
Recognize products of bacteria, virus and other pathogens ( almost all!!)
Results in production of mediators of inflammation
Inflammasome
- Multiprotein cytoplasmic complex
Recognize products of dead cells
Activation of Caspase-1
Activation of IL-1 which is the mediator of leukocyte recruitment.
These leukocytes phagocytose & destroy dead cells.
What are the changes in the vascular flow and caliber in acute inflammation
The first and the immediate change in the vessels is vasodilatation. This is due to the presence of histamine and initially it begins in arterioles. The vasodilatation results in increased blood flow and this is the reason for the redness/heat at the site of inflammation. Following vasodilatation is the increased vascular permeability which results in escape of fluid and proteins into the extravascular space, The mechanisms of which is described below.
The combined effect of vasodilatation and fluid loss results in slowing of blood in the vessel lumen, concentration of red blood cells and subsequently resulting increased viscosity. This results in engorgement of small vessels and is referred to as Stasis. This stasis is seen as vascular congestion in the site of inflammation.
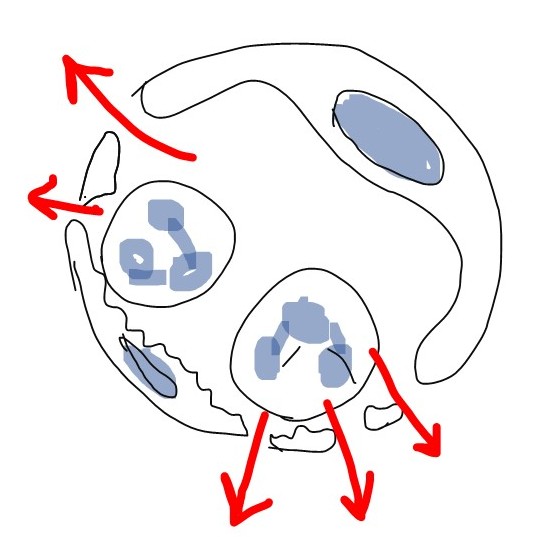
Discuss the mechanisms of Increased Vascular Permeability in acute inflammation
Increased vascular permeability is the Hallmark of Acute inflammation
Here, There is escape of fluid, blood cells and proteins from the blood vessels into the interstitial tissue
The mechanisms of increased vascular permeability are as below
Contraction of endothelial cells: this is the most common mechanism and it occurs immediately. This is short lived and hence also referred to as “ immediate transient response”. Histamine, bradykinin and leukotrienes are the chemical mediators responsible for this mechanism.
Direct damage to endothelium/Endothelial injury: Burns , microbes and toxins can directly damage the endothelial cells and through the gaps in the damaged endothelial cells, the fluid escapes. This also occurs immediately but this is sustained for several hours until the damage is repaired.
Endothelial injury due to leukocytes: The neutrophils themselves when they adhere to the vascular wall can damage the endothelial cells and again the fluid leaks through these damaged cells. This also occurs immediately but this is sustained for several hours until the damage is repaired.
Transcytosis: This mechanism involves the intracellular channels wherein there is increased transport of fluid and proteins. These channels are stimulated/activated by VEGF( Vascular endothelial growth factor) which promote leakage of the fluid and proteins. However, this mechanism in the context of acute inflammation is still unclear.
Click here to watch the Video tutorials of INFLAMMATION Part 1: General Concepts, Types, Vascular Changes in Acute Inflammation