Benign prostatic hyperplasia(BPH) / Nodular hyperplasia of prostate
Introduction:
BPH or benign prostatic hypertrophy or Nodular hyperplasia of prostate is a condition characterised by the enlargement of prostate especially in the peri-urethral regions of prostate, which is non-neoplastic in nature. This is more common in men above 50 years of age with its incidence approaching almost 80% in men above 80 years of age. Please see here the health benefits of using Prostadine supplement for prostate.
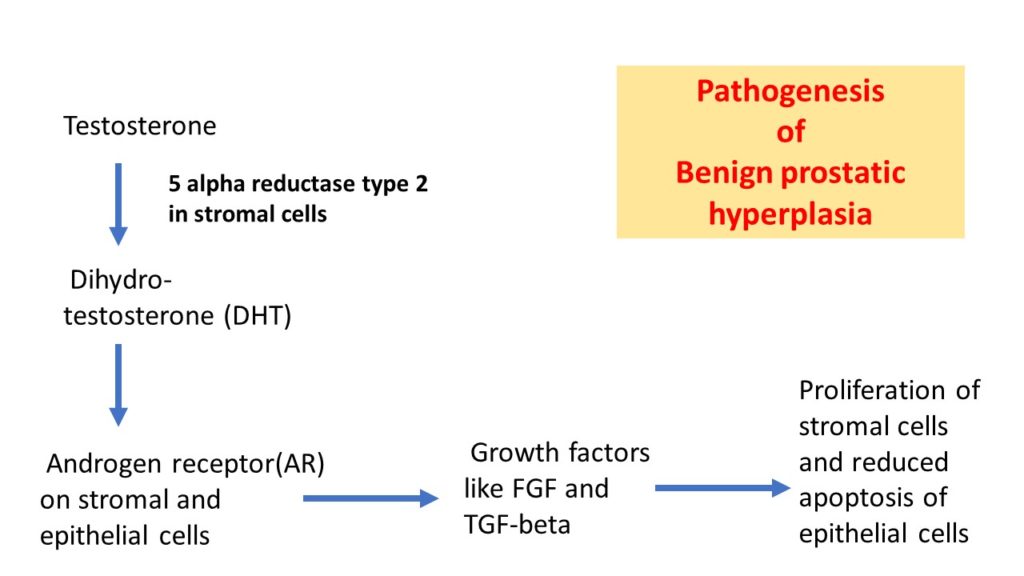
Pathogenesis:
The important mediator implicated in BPH pathogenesis is Dihydroxy-testosterone(DHT). This is produced by the stromal cells of prostate under the action of the enzyme 5alpha reductase type2 as shown in the reaction below. DHT is more potent than testosterone and forms a more stable complex with Androgen receptor on both stromal and epithelial cells of prostate. This complex stimulates the production of growth factors like the Fibroblast growth factor(FGF) and the Transforming growth factor beta(TGF-beta).
The exact pathogenesis is not known. It is thought to be the proliferation of stromal cells and the reduced apoptosis of epithelial cells under the action of gwoth factors like FGF and TGF-beta.
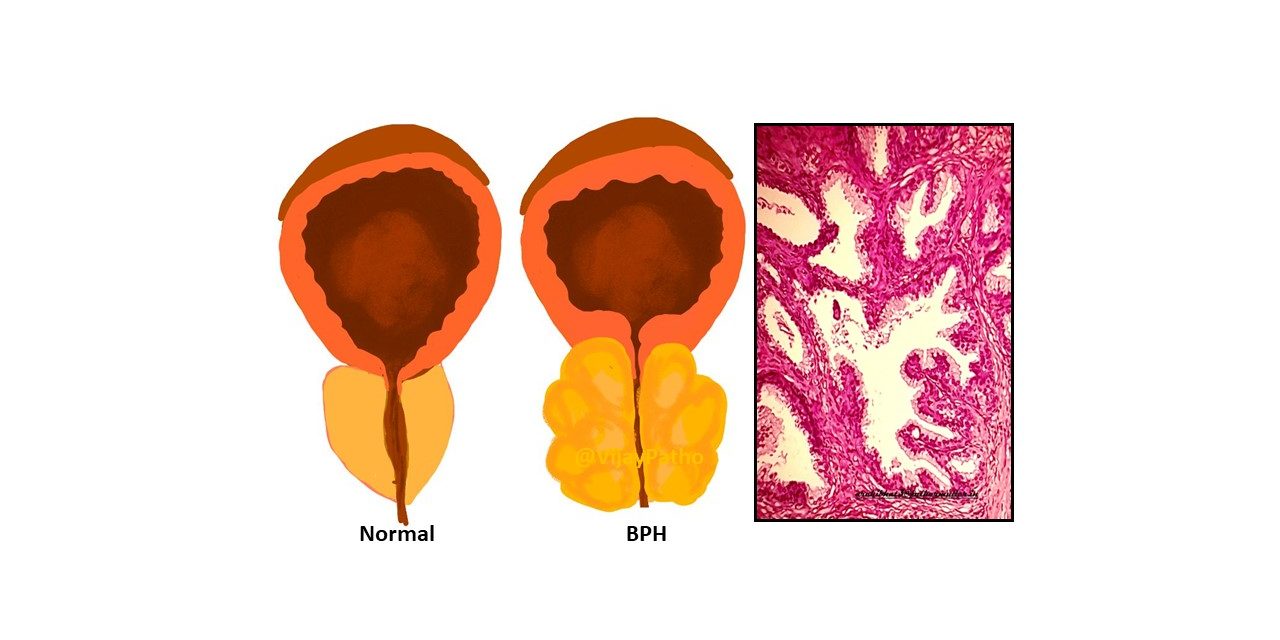
Morphology:
The prostate is enlarged with nodularity and weighs 60 to 100gm. The average normal weight of prostate is 20gm. The peri-urethral region is involved predominantly leading to the compression of the urethra. Median lobe hypertrophy refers to the nodular enlargement beneath the urethral mucosa projecting into the floor of urethra.
Gross pathology:
On gross examination, the nodules vary in size,colour and consistency from soft, yellow-pink to firm grey- white depending on predominance of epithelial or stromal cellularity respectively. The nodules do not have a capsule but they compress the surrounding prostatic tissue to form a thin rim around them.
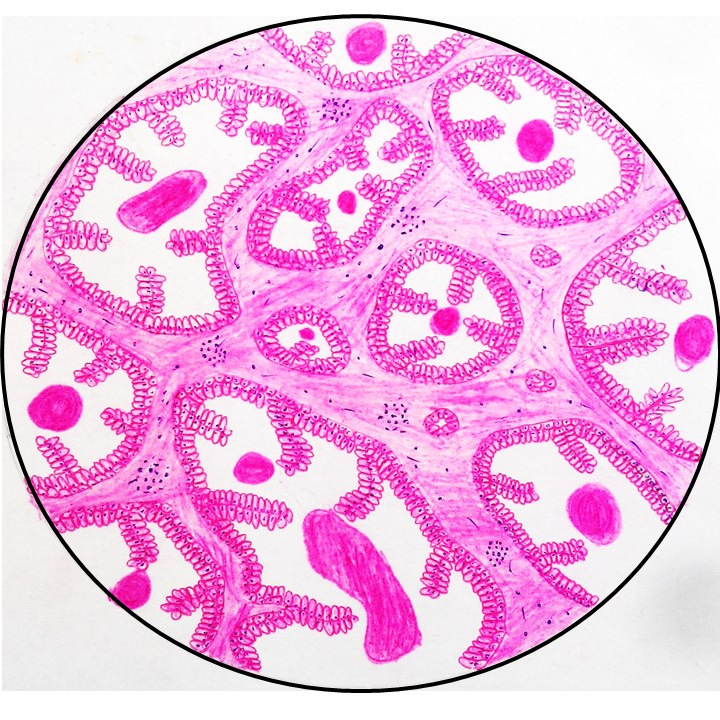
Microscopy :
The nodules on histopathological examination show prostatic glands of varying sizes lined by two layers of cells, the inner columnar and the outer cuboidal to flattened basal cell layers. Some of the glands show papillary infoldings. The lumen of the glands contains eosinophilic secretion called the corpora amylacea. Foci of squamous metaplasia and mild lymphocytic infiltrate can be seen.
Clinical features:
Most common clinical presentation is urinary obstruction. There is incomplete emptying of bladder which predisposes for recurrent urinary tract infections. Other symptoms include nocturia, difficulty in micturition and dysuria. In occasional cases, emergency catherization may be required to relieve acute urinary retention.
Treatment:
Medical therapy includes alpha- blockers and inhibitors of 5alpha reductase. Severe cases may require surgical treatment in the form of Transurethral resection of prostate(TURP) which is considered the gold standard. Other modalities of treatment include high intensity ultrasound, laser therapy, transurethral electrovaporization and transurethral radiofrequency needle ablation.