Infective Endocarditis Part 2: Morphology, Clinical Features & Diagnosis
What did we cover in Part 1 ( CLICK HERE) ?
In the first part, we learned that infective endocarditis is a microbial infection affecting the heart valves or mural endocardium, forming vegetations made of thrombotic debris and microbes. These vegetations often cause damage to the underlying heart tissue.
MORPHOLOGY OF INFECTIVE ENDOCARDITIS
What is the hallmark of infective endocarditis morphologically?
The classic feature is the presence of vegetations—bulky, friable, and destructive masses made up of:
Fibrin
Inflammatory cells
Bacteria or other organisms
Where are vegetations commonly found?
Most often on the aortic and mitral valves
In IV drug users, the right-sided valves (especially the tricuspid) are usually involved
On which part of the valve surface do vegetations form?
Vegetations tend to form on:
The atrial side of atrioventricular (AV) valves (mitral, tricuspid)
The ventricular side of semilunar valves (aortic, pulmonary)
These areas face the incoming jet of turbulent blood flow, which makes them prone to injury and microbial colonization.
What happens if vegetations are left untreated?
They can:
Erode into the myocardium forming an abscess, specifically a ring abscess around the valve annulus
Break off and embolize, causing septic infarcts throughout the body
How does morphology differ in subacute infective endocarditis?
Vegetations here may show signs of healing:
Granulation tissue at the base
Fibrosis, calcification, and chronic inflammation within the valve
CLINICAL FEATURES
What is the most common symptom of infective endocarditis?
Fever is the most frequent and sometimes the only presenting feature.
How does acute infective endocarditis present?
Sudden, stormy onset
Rapid development of:Fever,Chills, Weakness, Lethargy
Heart murmurs are present in up to 90% of cases with left-sided involvement
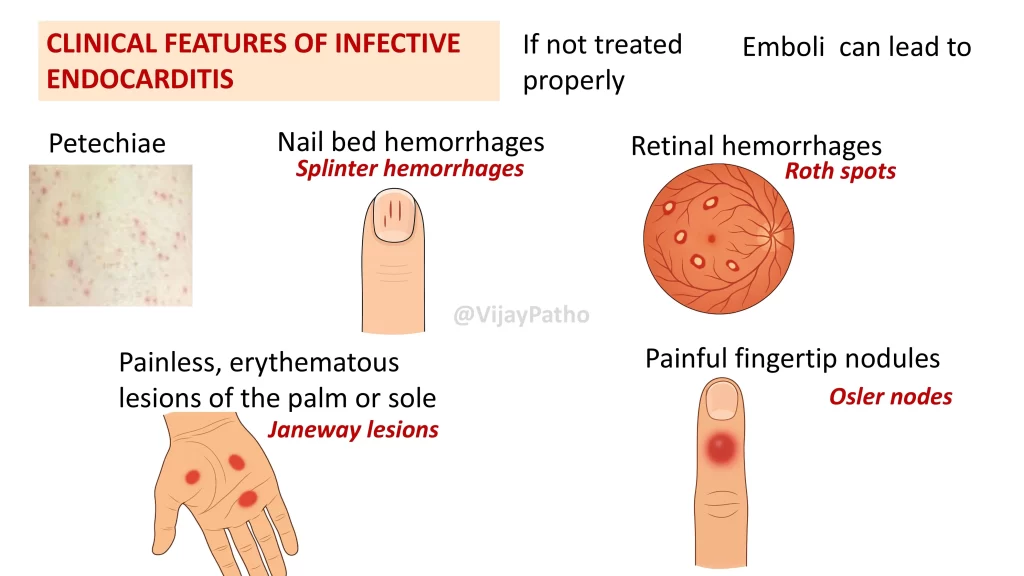
What are some key peripheral signs in acute cases?
Petechiae (tiny hemorrhages on the skin)
Splinter hemorrhages (nail bed bleeds)
Roth spots (retinal hemorrhages with pale centers)
Janeway lesions (painless red lesions on palms or soles)
Osler nodes (painful nodules on fingertips) — these are immunological reactions
What about subacute infective endocarditis?
Symptoms may be subtle or absent
Patients may show:
Fatigue
Weight loss
Flu-like symptoms
Night sweats
Anorexia
Splenomegaly may occur due to prolonged immune stimulation
In older adults, symptoms can be minimal or vague
COMPLICATIONS
What complications can occur in infective endocarditis?
These usually begin within the first few weeks:
Glomerulonephritis due to immune complex deposition
Sepsis
Arrhythmias
Septic emboli leading to infarcts in various organs
DIAGNOSIS
What is the most important investigation for diagnosis?
Blood cultures:
Positive in 90–95% of cases
If cultures are negative, it is termed culture-negative endocarditis, often due to prior antibiotic use or difficulty isolating deeply embedded organisms
What other investigations are helpful?
ECG: May show PR prolongation or bundle branch block if the conduction system is involved
Echocardiography: Helps detect vegetations and assess valve function
MODIFIED DUKE CRITERIA
What are the Modified Duke Criteria?
They’re used to establish a clinical diagnosis of infective endocarditis. There are two categories:
Pathologic criteria
Clinical criteria
What counts as pathologic criteria?
Demonstration of microorganisms on culture
Histological confirmation of active endocarditis from vegetations or intracardiac abscesses
If either is positive, the diagnosis is confirmed.
What are the clinical criteria?
Major criteria (any of the following):
Positive blood culture for typical or persistent organisms
Evidence of vegetations on echocardiography
New valvular regurgitation
Minor criteria (need at least 3 if only 1 major is present):
Predisposing condition or IV drug use
Fever
Vascular phenomena (e.g., hemorrhages)
Immunologic phenomena (e.g., Osler nodes, Roth spots)
Positive culture for an unusual organism
How do you make a clinical diagnosis?
A diagnosis is established if:
2 major criteria are met, or
1 major + 3 minor, or
5 minor criteria alone
PROGNOSIS
What is the prognosis for infective endocarditis?
If untreated, it is generally fatal. However, with:
Prompt antibiotic therapy and
Valve replacement (if needed),
outcomes significantly improve, and mortality is reduced.
Save this page or share it with your peers! Don’t forget to check out our video explanation if you haven’t already.