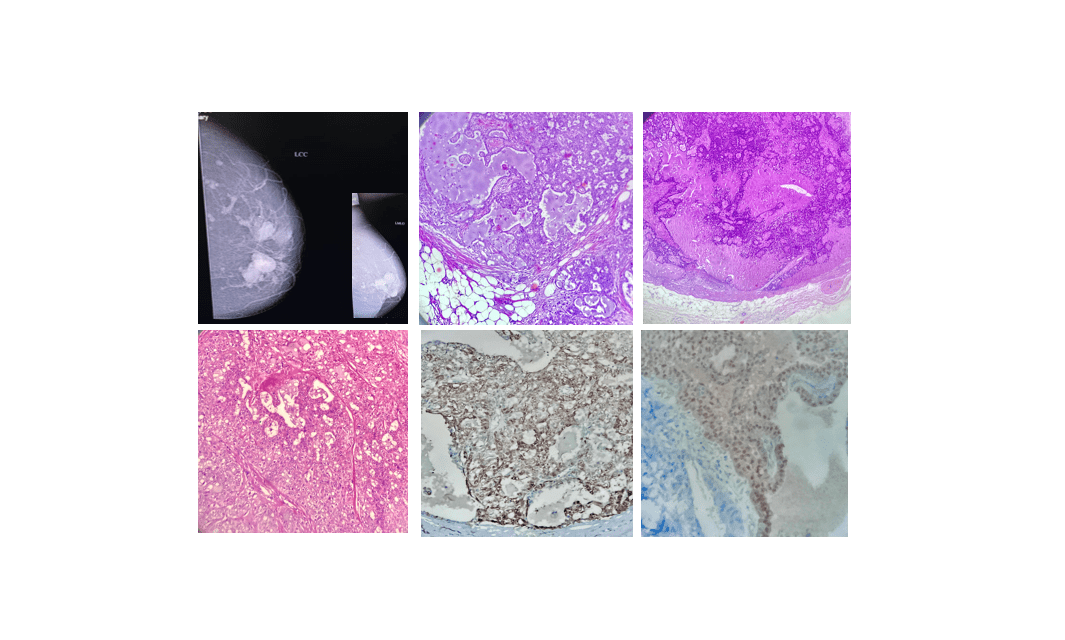
Pathology of Secretory Breast Carcinoma
Secretory breast carcinoma, originally referred to as “juvenile carcinoma,” was first identified by McDivitt and Stewart in 1966. It was later renamed by Tavassoli and Norris, who highlighted its unique features, including the presence of abundant secretory material.
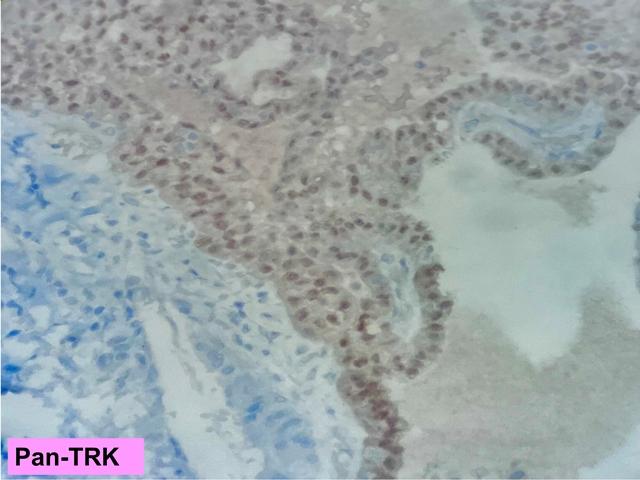
The use of a pan-TRK monoclonal antibody for immunohistochemistry aids in diagnosing the tumour with ETV6-NTRK3 gene mutation in cases of secretory carcinoma.
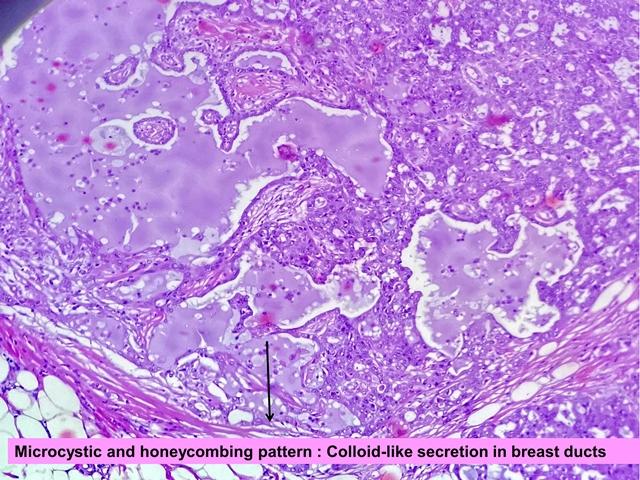
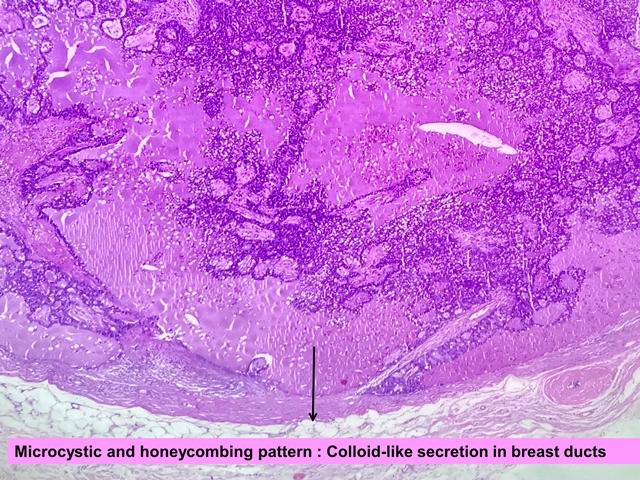
Microscopic features
The tumour cells are polygonal with eosinophilic granular or vacuolated cytoplasm and round to oval nuclei arranged in microcystic/honeycomb, solid, tubular or papillary growth patterns with the presence of ductal carcinoma in situ component. Microcystic areas simulate thyroid follicles and may merge to form small solid sheets and mixed pattern. Intracytoplasmic and extracellular eosinophilic or amphophilic secretions was present which are PAS positive.
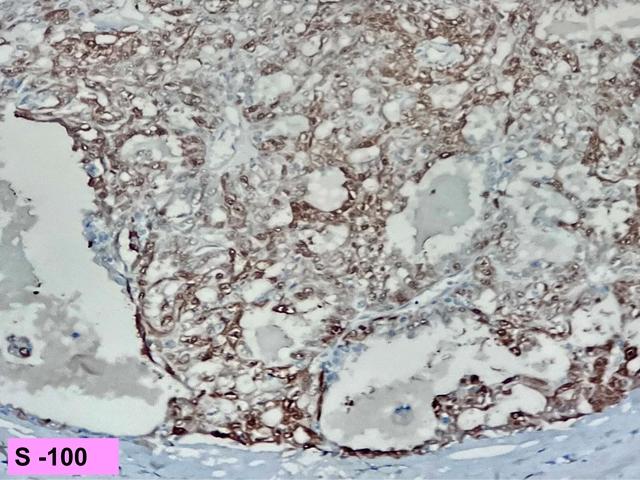
Immunohistochemically,
Strong and Diffuse Expression:
CEA (polyclonal)
S-100
Mammoglobin
SOX-10
MUC-4
Basal Markers (often expressed, sometimes in a focal pattern):
CK5/6
EGFR (HER 1)
Additional Positive Markers:
GATA-3
CK-8/18
CD117
Vimentin
Hormone Receptor Status:
Most cases are triple-negative for ER, PR, and HER-2
Some cases may show weak expression of ER/PR
Prognosis
Secretory carcinoma generally demonstrates indolent behavior. However, it has a propensity to recur unless completely excised. Local lymph node metastasis occurs in up to 22% of patients and distant metastasis, while rare, has been reported in a subset of cases.