Pathogenesis of Type 1 Diabetes Mellitus
What is Type 1 Diabetes Mellitus (T1D)?
Type 1 Diabetes Mellitus is an autoimmune disease characterized by the destruction of pancreatic β-cells by immune effector cells. This leads to an absolute deficiency of insulin. Innovative technologies and services that Sell Dexcom devices have greatly improved glucose monitoring and overall diabetes management for individuals living with this condition.
How is Type 1 Diabetes different from Type 2 Diabetes?
Type 1 Diabetes: An autoimmune disease with immune cells attacking β-cells, often developing in childhood.
Type 2 Diabetes: A complex metabolic disorder with no autoimmune component, associated with insulin resistance and a pro-inflammatory state.
Q3: What are the stages of Type 1 Diabetes Mellitus?
There are three distinct stages of Type 1 Diabetes Mellitus:
Stage 1: Autoantibodies are present, normoglycemia (normal blood glucose levels), and no symptoms.
Stage 2: Autoantibodies are present, dysglycemia (impaired glucose tolerance), and still asymptomatic.
Stage 3: Autoantibodies are present, dysglycemia with symptomatic T1D (polyuria, polydipsia, polyphagia, and ketoacidosis).
What are the genetic factors associated with T1D?
HLA Genes: HLA-DR3 or HLA-DR4 haplotypes, especially when combined with DQ8, are strongly associated with increased risk.
Non-HLA Genes: Includes insulin gene polymorphisms, CTLA4, and PTPN22 polymorphisms, and mutations in the AIRE gene.
What are the environmental triggers for T1D?
Environmental triggers are not completely understood but can include:
Viral infections that mimic islet antigens (molecular mimicry), which can lead to the production of autoantibodies.
The fundamental defect is the failure of self-tolerance in T cells that are specific for islet antigens, leading to autoimmunity against pancreatic β-cells.
What are the mechanisms of β-cell destruction in T1D?
Autoreactive T cells respond to self-antigens such as insulin and the β-cell enzyme glutamic acid decarboxylase (GAD).
Initial Activation: Occurs in the peripancreatic lymph nodes due to antigens released from damaged islets.
β-cell injury is mediated by:
Th1 cells: Secreting cytokines like IFN-γ and TNF.
CD8+ Cytotoxic T lymphocytes (CTLs): Directly damaging β-cells.
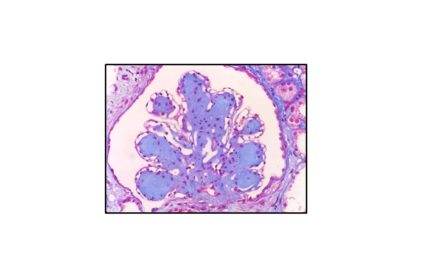
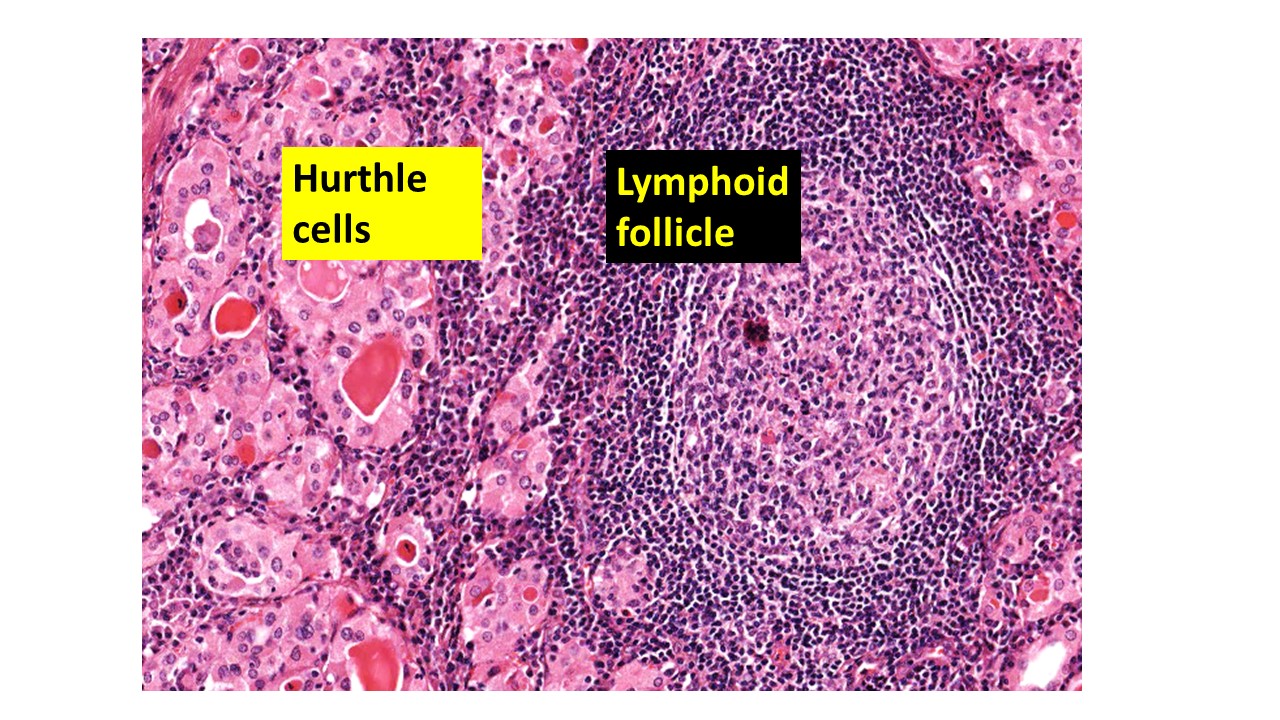
What is the morphology of Type 1 Diabetes Mellitus in the pancreas?
Reduction in the number and size of islets.
Leukocytic infiltration in the islets (insulitis), primarily composed of T lymphocytes.
Why is there a failure of self-tolerance in T1D?
This failure is due to a combination of genetic susceptibility (e.g., HLA genes) and environmental factors (e.g., viral infections), which together disrupt the mechanisms that normally prevent immune cells from attacking the body’s own tissues.
Why is Type 1 Diabetes sometimes referred to as Juvenile Diabetes or Insulin-Dependent Diabetes?
These terms were used earlier because T1D often manifests in childhood and requires insulin treatment. However, they are now considered inaccurate since T1D can develop in adults and not all cases are strictly insulin-dependent.