Myocardial Infarction: Pathogenesis and Infarct Types
What is myocardial infarction (heart attack)?
Myocardial infarction refers to the death of cardiac muscle due to prolonged ischemia. It is commonly known as a heart attack.
Myocardial infarction can occur at any age. Around 10% of cases are seen in people under 40 years, and about 45% in those under 65 years. The prevalence increases with age. Men are more commonly affected than women during reproductive years due to estrogen’s protective effect. However, the incidence rises in postmenopausal women as estrogen levels decline.
Which coronary arteries are commonly involved in myocardial infarction?
The three major coronary arteries implicated in myocardial infarction are:
Right coronary artery (RCA)
Left anterior descending (LAD) coronary artery
Left circumflex artery (LCX)
What is the primary cause of myocardial infarction?
In 90% of cases, obstructive atherosclerotic lesions in the coronary arteries are the primary cause. These lesions typically form in the epicardial arteries.
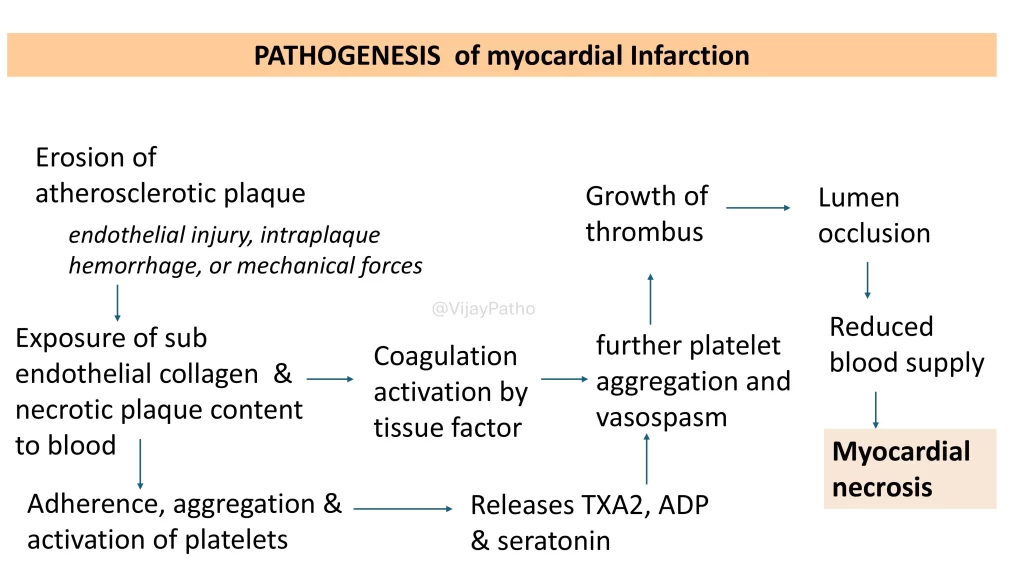
How do atherosclerotic plaques lead to obstruction?
Plaque erosion occurs due to:
Endothelial injury
Intralesional hemorrhage
Mechanical forces
Once plaques erode, subendothelial collagen and necrotic plaque contents are exposed to the blood. This exposure triggers platelet adherence and aggregation, along with the release of mediators like thromboxane A2, ADP, and serotonin, causing vasospasm.Activation of tissue factor, initiates the coagulation cascade.
These events lead to thrombus growth, luminal occlusion, reduced blood supply, and myocardial necrosis.
What are other causes of myocardial infarction?
The remaining 10% of cases may result from:
Coronary emboli (e.g., from atrial fibrillation, mural thrombus, vegetations, or prosthetic material)
Vascular spasm (often drug-induced, e.g., cocaine)
Myocardial vessel inflammation (vasculitis)
Rare conditions like sickle cell disease, aortic dissection, or congenital coronary artery anomalies
What is the pathogenesis of myocardial infarction?
When blood flow is obstructed, oxygenation of myocardial tissue decreases. This leads to:
Reduced ATP production (earliest biochemical change).
Accumulation of metabolic waste products like lactic acid.
Impaired myocardial contractility, causing systolic dysfunction.
Ultrastructural changes such as myofibrillar relaxation, glycogen depletion, and mitochondrial swelling. These changes are reversible if blood flow is restored.
What happens if ischemia persists?
Severe ischemia (blood flow <10% of normal) for 20-30 minutes or longer causes irreversible myocardial necrosis.
It takes about 20 minutes for myocardial cells to die, emphasizing the importance of rapid diagnosis.
What are the time-dependent changes in myocardial cells after obstruction?
Seconds: Onset of ATP depletion.
<2 minutes: Loss of contractility.
10 minutes: ATP reduced to 50% of normal.
40 minutes: ATP reduced to 10% of normal.
20-40 minutes: Irreversible cell injury starts, with membrane damage and leakage of cellular contents.
>1 hour: Microvascular injury begins, further worsening ischemia.
How is early myocardial necrosis detected?
The earliest detectable feature is the loss of sarcolemmal membrane integrity, leading to leakage of intracellular macromolecules like troponin and CK-MB into the bloodstream. These markers are used for early diagnosis.
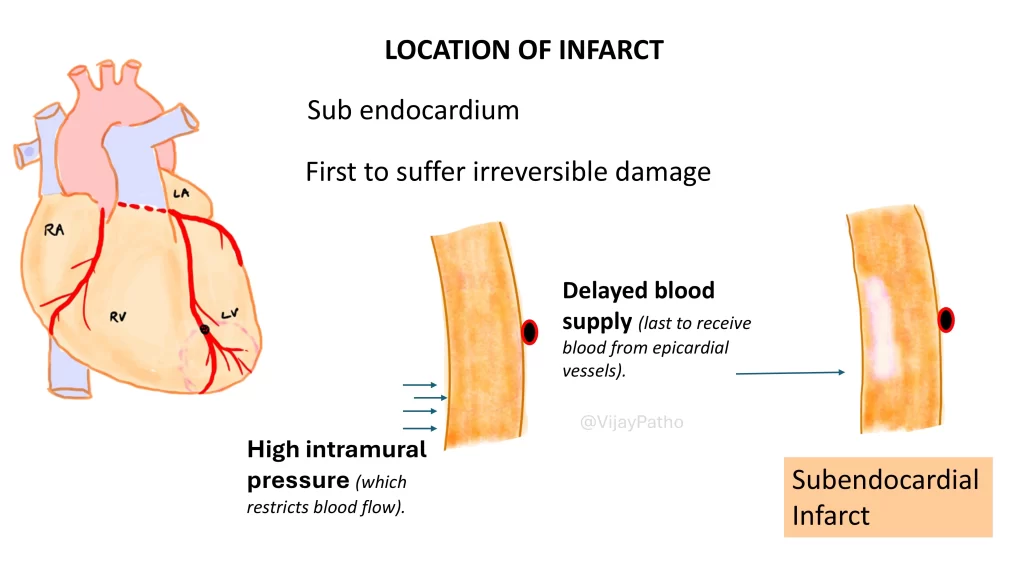
Where does infarction begin, and how does it progress?
The subendocardium is the first region to suffer irreversible damage because it is the last to receive blood and experiences high intramural pressure.
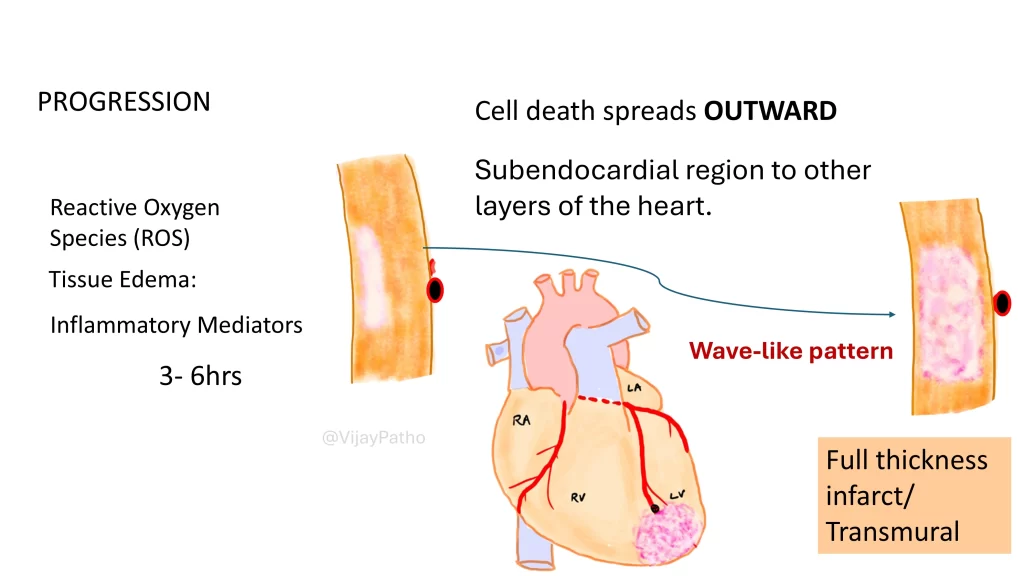
If untreated, the infarction progresses outward from the subendocardium to the epicardium over 3-6 hours, resulting in a transmural infarction (full-thickness infarction).
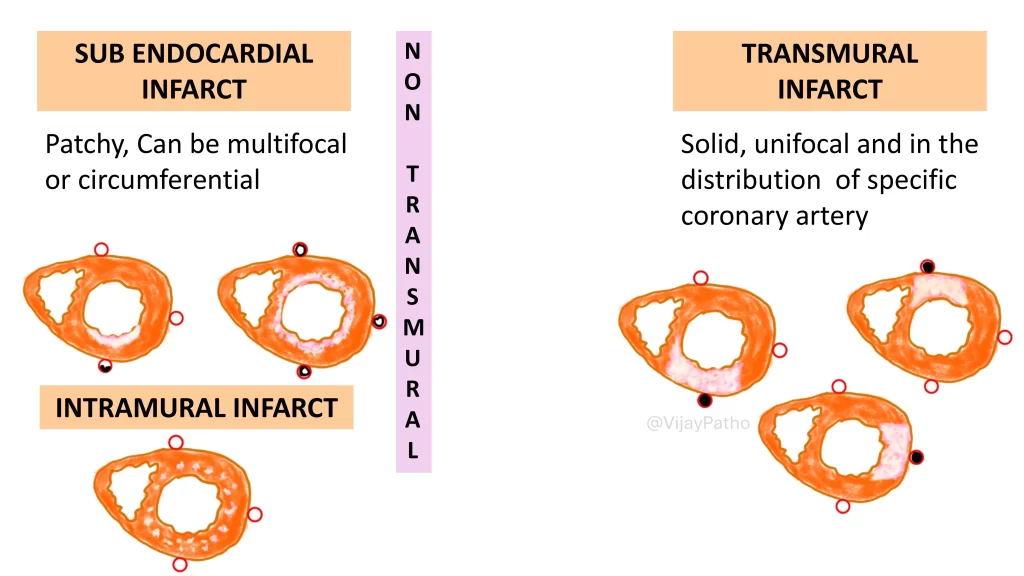
What are the types of infarction?
Subendocardial Infarction:
Limited to the inner one-third or half of the myocardium.
Can be patchy, multifocal, or circumferential (e.g., in global hypoperfusion/shock).
Does not cause wall weakening or aneurysm formation.
Transmural Infarction:
Affects the full thickness of the myocardium in the distribution of a specific coronary artery.
Associated with solid, unifocal infarcts.
Can lead to complications like aneurysms or ventricular rupture.
What are the key differences between subendocardial and transmural infarcts?
As illustrated below
CLICK BELOW to watch the video tutorial on pathogenesis of myocardial infarction