Understanding the Complications of Myocardial Infarction (Heart Attack)
What is the in-hospital death rate for myocardial infarction?
The in-hospital death rate is around 7-8%. For ST-segment elevation myocardial infarction (STEMI), it’s about 10%, while for non-ST segment elevation myocardial infarction (NSTEMI), it’s around 6%.
What is the death rate for myocardial infarction outside the hospital?
About one-third of patients die outside the hospital, mainly due to arrhythmia within the first hour.
What percentage of patients experience complications after an acute myocardial infarction?
Around 75% of patients experience one or more complications.
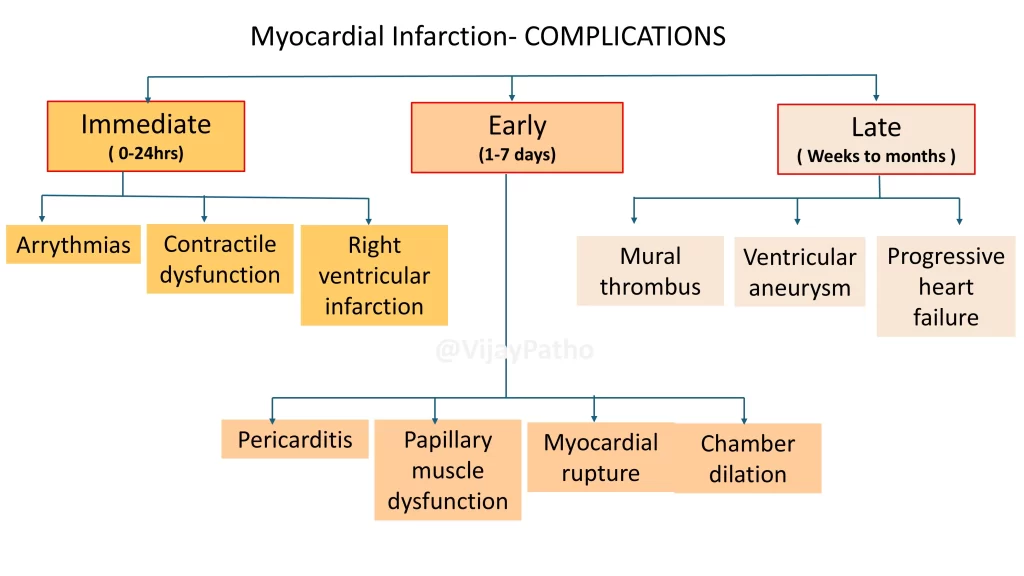
How are complications classified based on time?Complications are classified as:
Immediate (within 24 hours): Arrhythmias, contractile dysfunction, and right ventricular infarction.
Early (1 to 7 days): Pericarditis, papillary muscle dysfunction, myocardial rupture, and chamber dilation.
Late (after 1 week): Mural thrombus, ventricular aneurysm, and progressive heart failure.
Why do arrhythmias occur after a myocardial infarction?
The infarcted myocardium becomes irritable, leading to conduction disturbances like heart block, bradycardia, supraventricular tachycardia, and ventricular tachycardia. Ventricular fibrillation is the most serious and usually occurs within the first hour.
What causes contractile dysfunction after myocardial infarction?
Weakened myocardial tissue reduces the heart’s ability to pump blood, causing hypotension, pulmonary congestion, and pulmonary edema. Severe cases can lead to cardiogenic shock, especially if more than 40% of the left ventricle is damaged.
How common is right ventricular infarction and what are its effects?
Isolated right ventricular infarction occurs in 1-3% of cases, usually due to right coronary artery occlusion. It leads to right-sided heart failure and systemic hypotension due to blood pooling in the venous circulation.
What causes pericarditis after myocardial infarction?
Myocardial inflammation can irritate the overlying epicardium, causing fibrinohemorrhagic pericarditis. It usually appears 2-3 days after the infarction, causing chest pain and a pericardial friction rub. Extensive pericarditis can cause large effusions or dense adhesions, leading to constrictive heart disease.
What is Dressler syndrome?
Dressler syndrome is a delayed form of pericarditis that occurs 2-10 weeks after myocardial infarction due to the formation of antibodies against myocardial tissue.
What is papillary muscle dysfunction and what are its effects?
Papillary muscle dysfunction occurs due to ischemia, weakening the muscle and leading to mitral regurgitation because the mitral valve cannot close properly.
What are the types of myocardial rupture and their consequences?
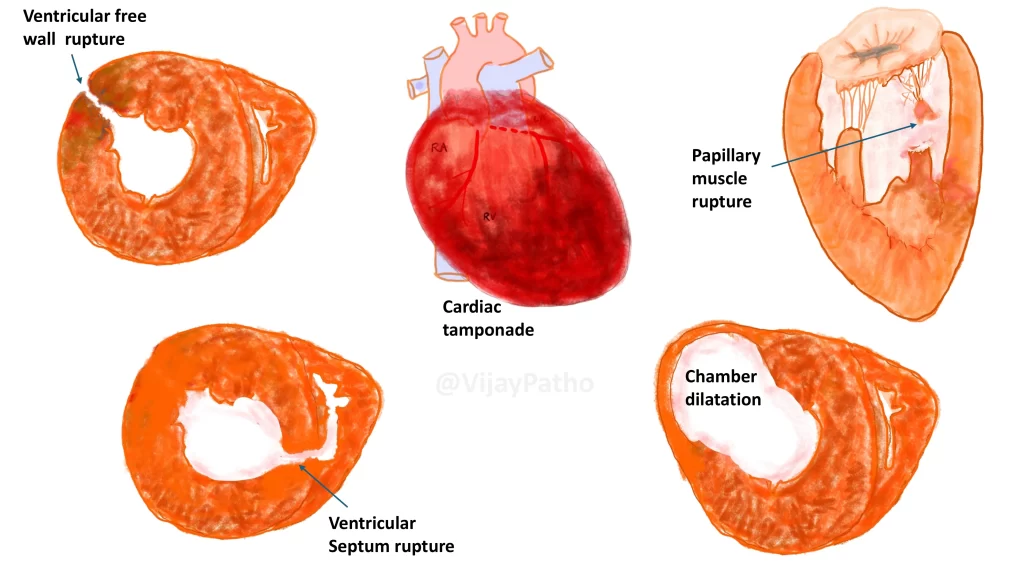
Myocardial rupture occurs in 1-5% of cases, typically between the 3rd and 7th day when the myocardial wall is weakest. Types include:
Ventricular free wall rupture: The most common type, causing blood to leak into the pericardium, leading to hemopericardium and cardiac tamponade.
Ventricular septal rupture: Creates a ventricular septal defect with left-to-right shunting.
Papillary muscle rupture: Leads to severe mitral regurgitation.
What is chamber dilation and why does it occur?
Chamber dilation happens when necrotic muscle stretches and thins out, causing disproportionate dilation of the infarcted area.
What causes mural thrombus formation?
Inflammation of the endocardium makes the surface thrombogenic, promoting platelet adhesion and fibrin deposition. Reduced myocardial contractility causes blood stasis, further increasing the risk of thrombus formation, which can lead to left-sided thromboembolism.
What is a ventricular aneurysm and how does it form?
A ventricular aneurysm develops in about 10-15% of transmural infarctions when scar tissue causes the ventricular wall to bulge outward. True aneurysms are composed of myocardial tissue, while false aneurysms occur when a rupture is walled off by a blood clot.
Why are ventricular aneurysms dangerous?
The damaged muscle around an aneurysm can cause irregular electrical conduction, leading to ventricular tachycardia.
What leads to progressive heart failure after myocardial infarction?
Over time, the weakened myocardial wall and cumulative effects of complications result in progressive heart failure.
CLICK below to watch the video tutorial on complications of myocardial infarction