What is medullary thyroid carcinoma?
A: Medullary thyroid carcinoma (MTC) is a form of cancer originating from the parafollicular cells (C cells) of the thyroid gland. These cells are known for producing the hormone calcitonin. MTC is a neuroendocrine tumor, accounting for about 1 to 2% of thyroid cancers.
Q: How is medullary thyroid carcinoma classified?
A: MTC is classified based on its origin from parafollicular cells. MTC can be either sporadic or familial, with familial cases sometimes associated with multiple endocrine neoplasia syndromes (MEN 2A or 2B).
Q: How does the epidemiology of sporadic and familial medullary thyroid carcinoma differ?
A: Sporadic MTC, which is the most common form, typically occurs in adults in the fifth to sixth decades of life. In contrast, familial MTC, often associated with multiple endocrine neoplasia syndromes, is more likely to be diagnosed in children and young adults.
Q: What is the pathogenesis of medullary thyroid carcinoma?
A: The pathogenesis of MTC involves gain-of-function driver mutations in the RET proto-oncogene, a receptor tyrosine kinase. These mutations are crucial in both sporadic and familial forms of MTC.
A: How does medullary thyroid carcinoma present clinically?
A: Clinically, MTC commonly presents as a neck mass, typically in the upper two-thirds of the thyroid lobes. Patients may experience compression symptoms like dysphagia, hoarseness, or dyspnea. Hormonal effects such as diarrhea can occur due to secretion of vasoactive amines. Elevated serum calcitonin levels are a key diagnostic marker.
A: What diagnostic methods are used for medullary thyroid carcinoma?
A: The diagnosis of MTC often begins with an ultrasound of the neck when a mass is detected. Fine-needle aspiration cytology (FNAC) is then performed, which can typically diagnose MTC. Additionally, molecular diagnostic tests can identify RET mutations, further confirming the diagnosis.
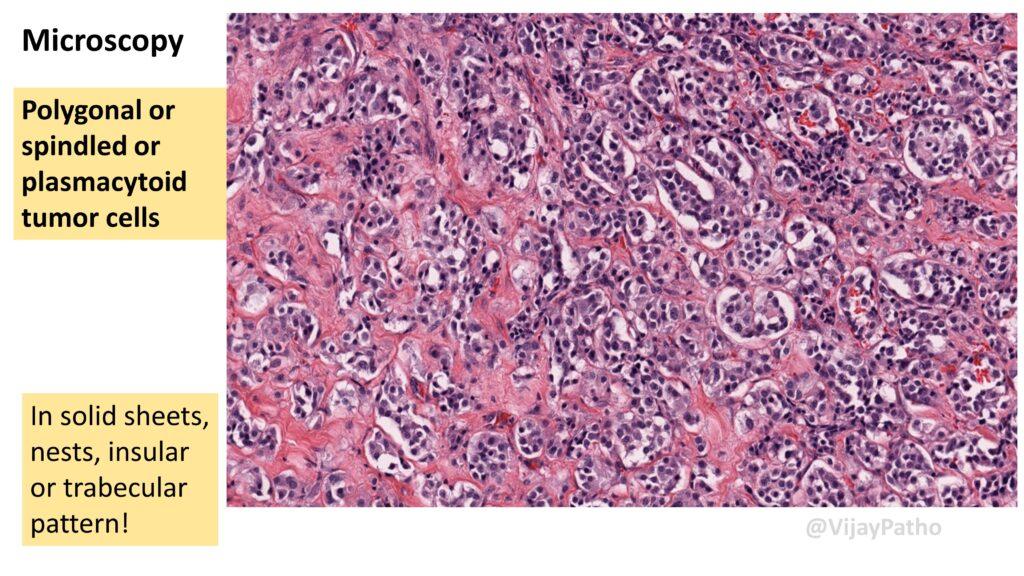
Q: What are the morphological characteristics of medullary thyroid carcinoma?
A: Grossly, sporadic MTC usually presents as a solitary nodule, predominantly in the upper two-thirds of one thyroid lobe. In contrast, familial MTC, often associated with multiple endocrine neoplasia syndromes, tends to present as bilateral and multifocal lesions.
Medullary thyroid carcinoma (MTC) is characterized microscopically by polygonal, spindle-shaped, or plasmacytoid cells. These cells can form various patterns, including solid sheets, nests, insular, or trabecular patterns. A notable feature of MTC is the presence of amyloid in the stroma, which results from the overproduction of calcitonin.
Q: What is the significance of calcitonin in the pathology of medullary thyroid carcinoma?
A: Calcitonin, produced by the C cells or parafollicular cells in MTC, is significant for both the pathology and clinical management of the disease. Elevated levels of calcitonin in the blood are a key diagnostic marker for MTC. Additionally, the overproduction of calcitonin leads to the characteristic amyloid deposition in the tumor’s stroma, aiding in the histopathological diagnosis.
Q: What are the special stains or techniques used in the pathology of medullary thyroid carcinoma?
A: The Congo red stain is used to identify amyloid in the stroma, which is a distinctive feature of MTC. Under polarized light, the amyloid stained with Congo red exhibits apple-green birefringence.
Additionally, immunohistochemical staining for calcitonin can be used to confirm the diagnosis, as MTC cells typically show strong positivity for this hormone.
CLICK HERE View the video tutotial