Diabetes Mellitus: Chronic Complications and Pathogenesis
What are chronic complications of diabetes mellitus?
Chronic complications refer to the long-term effects of persistent hyperglycemia in patients with diabetes, whether type 1 or type 2. These complications involve damage to large and medium-sized arteries (macrovascular disease) and small blood vessels (microvascular disease).
What are the types of chronic complications in diabetes?
Macrovascular complications: Accelerated atherosclerosis leading to an increased risk of myocardial infarction, stroke, and peripheral arterial disease.
Microvascular complications: Damage to the retina (diabetic retinopathy), kidneys (diabetic nephropathy), and peripheral nerves (diabetic neuropathy).
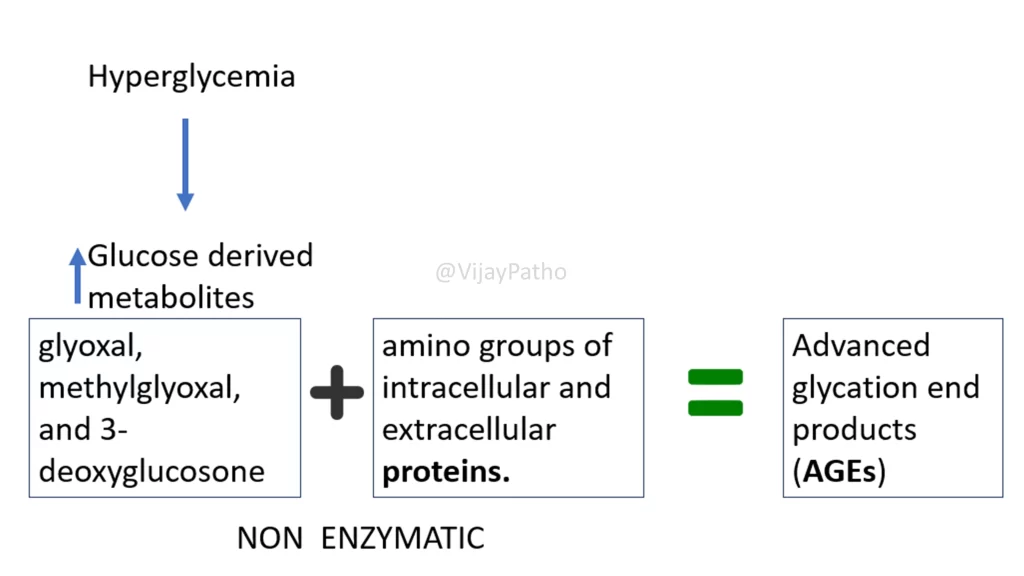
Chronic hyperglycemia leads to the formation of harmful glucose-derived metabolites, such as glyoxal and methylglyoxal. These combine with proteins in a non-enzymatic process to form advanced glycation end-products (AGEs), a major contributor to both microvascular and macrovascular complications.
What are advanced glycation end-products (AGEs), and how do they contribute to complications?
AGEs are molecules formed when glucose-derived metabolites bind to proteins. They can:
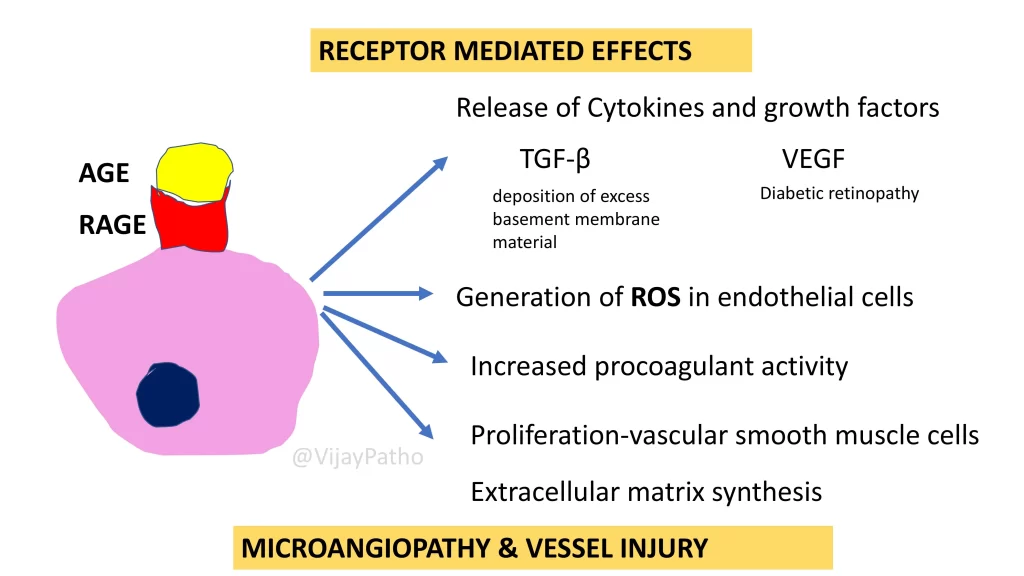
Act through receptors (RAGE): Receptors for AGEs are present on macrophages, endothelial cells, and vascular smooth muscle cells. When AGEs bind to RAGE, they trigger:
Cytokine and growth factor release (e.g., TGF-β and VEGF), leading to basement membrane thickening and diabetic retinopathy.
Reactive oxygen species generation, procoagulant activity, and vascular smooth muscle proliferation, causing blood vessel damage.
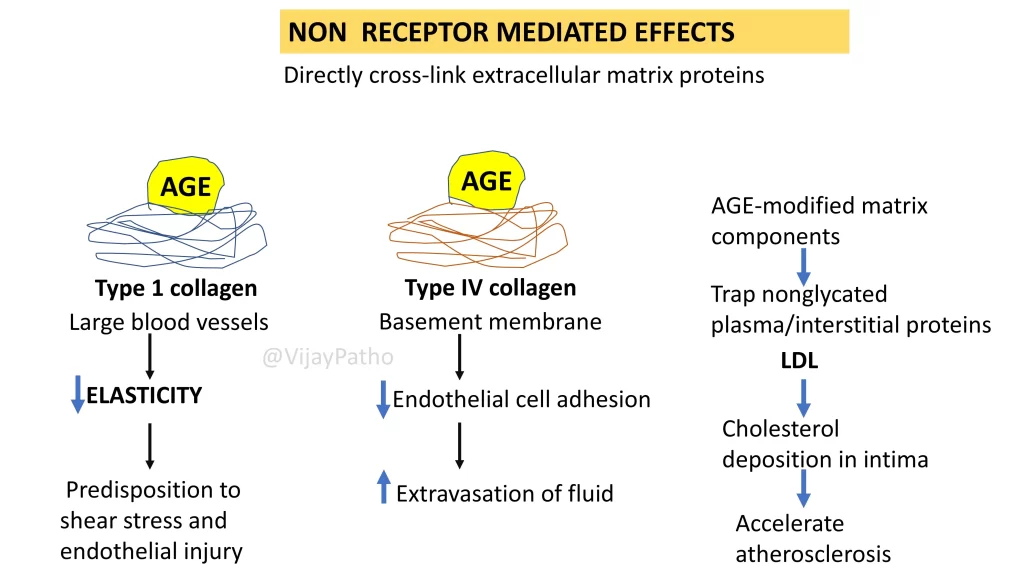
Act without receptors: AGEs crosslink extracellular matrix proteins, such as:
Type I collagen: Reduces elasticity in large blood vessels, predisposing to endothelial injury and atherosclerosis.
Type IV collagen: Impairs endothelial adhesion, increasing fluid leakage and contributing to microangiopathy.
How do AGEs contribute to atherosclerosis?
AGEs trap plasma proteins like LDL, leading to cholesterol deposition in vessel walls and accelerating atherosclerosis. This process makes diabetic patients more prone to cardiovascular events.
What is the role of the renal vasculature in chronic complications?
In the kidneys, AGEs cause basement membrane thickening by:
Trapping albumin and other proteins in the glycated basement membrane.
Inducing TGF-β release, which promotes excessive basement membrane deposition. This leads to microangiopathy and nephropathy.
What is protein kinase C (PKC) activation, and how does it contribute to complications?
Hyperglycemia activates PKC by increasing intracellular diacylglycerol. PKC activation results in:
Release of VEGF, TGF-β, and procoagulant factors, exacerbating microangiopathy.
How does oxidative stress occur in diabetes?
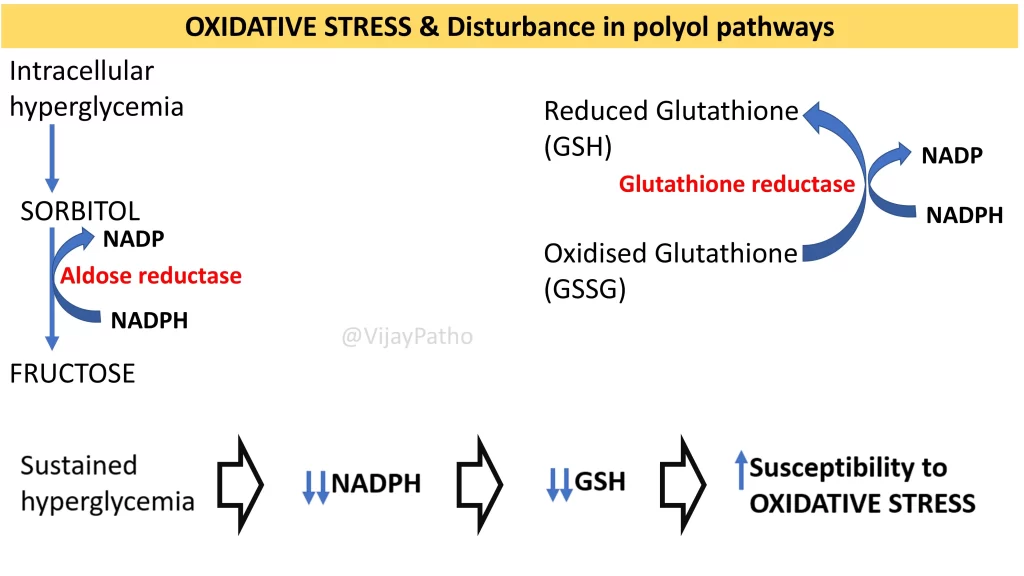
Intracellular hyperglycemia increases glucose metabolism through the polyol pathway, converting glucose to sorbitol and then fructose. This process depletes NADPH, reducing glutathione production. Since glutathione is a key antioxidant, its depletion makes cells more susceptible to oxidative damage.
What are the key mechanisms underlying chronic complications in diabetes?
Formation of AGEs and their receptor-mediated and non-receptor-mediated effects.
PKC activation leading to vascular dysfunction.
Oxidative stress caused by polyol pathway activation and reduced antioxidant defenses.
What are the clinical outcomes of these mechanisms?
Macrovascular disease: Atherosclerosis, myocardial infarction, and stroke.
Microvascular disease: Retinopathy, nephropathy, and neuropathy.
Summary: Chronic complications of diabetes result from persistent hyperglycemia leading to AGE formation, PKC activation, and oxidative stress. These mechanisms damage both large and small blood vessels, causing macrovascular and microvascular complications.
CLICK BELOW to watch the video tutorial on pathogenesis of chronic complications of diabetes mellitus