Infective Endocarditis Part 1: Risk Factors and Pathogenesis
What is infective endocarditis?
Infective endocarditis is a microbial infection that affects the inner lining of the heart, especially the heart valves or the mural endocardium. This infection leads to the formation of vegetations — clumps made up of thrombotic debris and microbes — which can damage the underlying heart tissues.
Why is it also called bacterial endocarditis?
Because in most cases, infective endocarditis is caused by bacteria. However, fungi and other microbes can also be responsible.
How is infective endocarditis classified?
There are two major types:
Acute infective endocarditis: A sudden, aggressive infection often affecting previously normal heart valves. It is caused by highly virulent organisms like Staphylococcus aureus.
Subacute infective endocarditis: A slower, less aggressive infection that usually affects already damaged or deformed valves. It’s typically caused by low-virulence organisms like Streptococcus viridans.
Acute cases rapidly destroy heart tissues and often require surgical intervention.Subacute cases are usually manageable with antibiotics alone. However, many cases fall somewhere in between these two extremes.
RISK FACTORS
What are the risk factors for developing infective endocarditis?
They can be broadly divided into two groups:
1. Cardiac causes
Rheumatic heart disease
Mitral valve prolapse
Bicuspid aortic valve
Calcified (stenotic) valves
Prosthetic heart valves
2. Host-related causes
Old age
Immunocompromised states (e.g., neutropenia, immunodeficiencies)
Cancer
Diabetes
Pregnancy
Alcoholism
Intravenous (IV) drug abuse
What role does transient bacteremia play?
Transient bacteremia — a temporary presence of bacteria in the bloodstream — is crucial. It allows the microbes to reach and attach to heart valves.
Common causes of transient bacteremia include:
Dental procedures
Urinary catheterization
Endoscopic procedures
COMMON CAUSATIVE ORGANISMS
Which organisms are commonly responsible?
Staphylococcus aureus
Most common in healthcare settings and IV drug users
Highly virulent — affects both healthy and damaged valves
Usually causes acute infective endocarditis
Streptococcus viridans
Common in community-acquired cases (50–60%)
Less virulent — often causes subacute endocarditis
Enterococci
Also a frequent culprit
What is the HACEK group?
HACEK organisms are a group of normal oral flora that can also cause endocarditis:
Haemophilus
Actinobacillus
Cardiobacterium
Eikenella
Kingella
Are there other organisms involved?
Yes, rarely, gram-negative bacilli and fungi may be responsible. Interestingly, in about 10% of cases, no specific causative organism is identified.
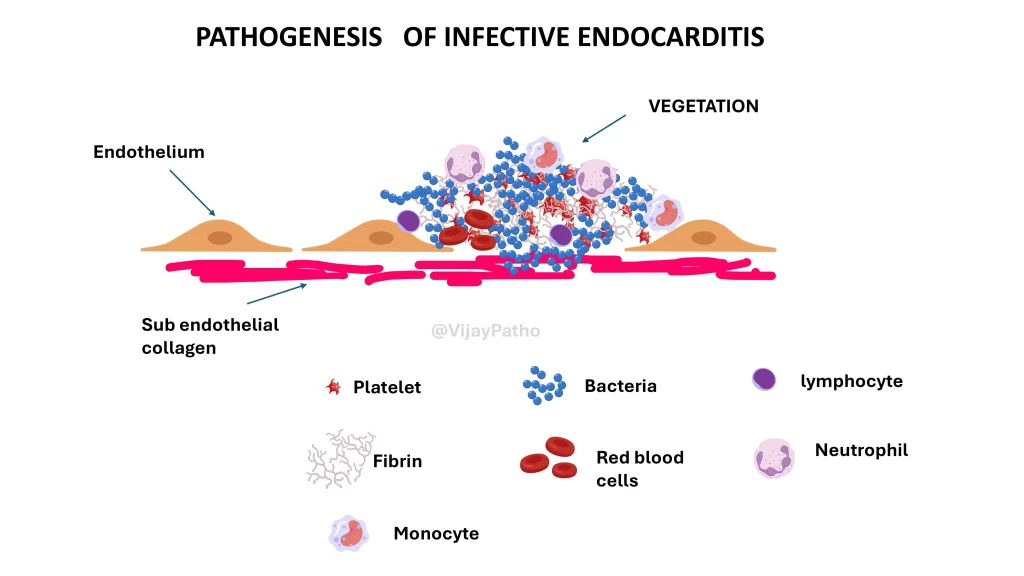
PATHOGENESIS OF INFECTIVE ENDOCARDITIS
What are the four key steps in the pathogenesis?
Endothelial damage
Pathogen entry into bloodstream
Pathogen adherence to the damaged site
Microbial proliferation and vegetation formation
Step 1: How does endothelial damage occur?
The endothelium (inner lining of the heart) normally resists infection. But when it’s damaged — due to turbulent blood flow, autoimmune diseases, or inflammation (e.g., rheumatic carditis) — it exposes the underlying collagen and subendothelial tissue.
Where is this damage most commonly seen?
At the points where heart valves close
On the upstream (inflow-facing) side of valves:
Atrial side of mitral and tricuspid valves
Ventricular side of aortic and pulmonary valves
Step 2: How does the pathogen enter the bloodstream?
Through common procedures like:
Dental work
Catheterization
Endoscopy
These allow microbes to enter circulation — a condition known as transient bacteremia.
Step 3: How do microbes adhere to the damaged site?
Once bacteria are in the bloodstream, they adhere to the damaged valves or the sterile thrombus (a clot formed without infection).
Factors aiding adherence include:
Upregulation of adhesion molecules (VCAM, ICAM-1, E-selectin)
Bacterial fibronectin-binding proteins
Extracellular polysaccharides that help bacteria stick to surfaces
Step 4: What happens after adherence?
The microbes begin to multiply, forming vegetations — masses made up of:
Platelets
Fibrin
Leukocytes
Red blood cells
Microorganisms
Why are vegetations dangerous?
They can locally destroy the heart tissue
Break off and form septic emboli
Cause valve perforation and lead to regurgitation
TAKEAWAY
Infective endocarditis is a serious heart infection that can be acute or subacute depending on the organism involved and the host’s heart condition. Key to its development is a combination of endothelial damage and the presence of microbes in the bloodstream. Understanding the pathogenesis helps in early diagnosis and management
share it with your friends, and don’t forget to subscribe to our YouTube channel for high-yield pathology tutorials!
watch the video tutorial below