Uterine Leiomyoma: These are the benign tumors of smooth muscle of uterus. They are most common tumors in females.
Uterine leiomyomas are commonly referred to as Fibroids.
Leiomyomas can occur in any age group but more common in 30 to 50 years. The incidence decreases after menopause.
Etiology: Exact etiology is not known, however age of menarche and parity are important risk factors. Earlier age of menarche and nulliparous women have higher risk.
Obesity, lack of exercise are also risk factors for development of leiomyomas.
Most important risk factor is exposure to environmental estrogens before puberty. This will result in hyper responsivenesness to normal levels of estrogen in adults.
Cytogenetic abnormalities: 40 to 50% of uterine leiomyomas show karyotypic abnormalities. The most common abnormalities are translocations on chromosome 12; deletion on chromosomes 3q and 7q.
Genes involved : HGMA2, ESR2, RAD5 & MED12
Clinical features:
Most often asymptomatic. But can manifest with abnormal uterine bleeding which is more common in submucosal leiomyomas. They can also interfere in fertility. Larger tumors result in various pressure symptoms
Morphology:
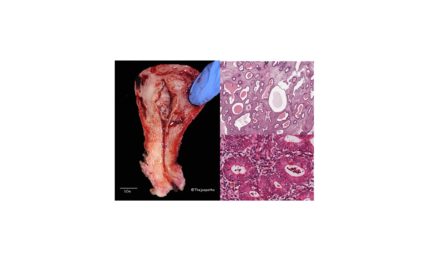
Gross:
These are usually multiple with sizes ranging from microscopic foci to large bulky tumors.
The cut surfaces are well circumscribed, with greywhite and whorled cut surface. They can be single or multiple. If the tumor is very large, the degenerative changes can be seen.
Highly cellular variant and lipoleiomyomas will be yellowish in color.
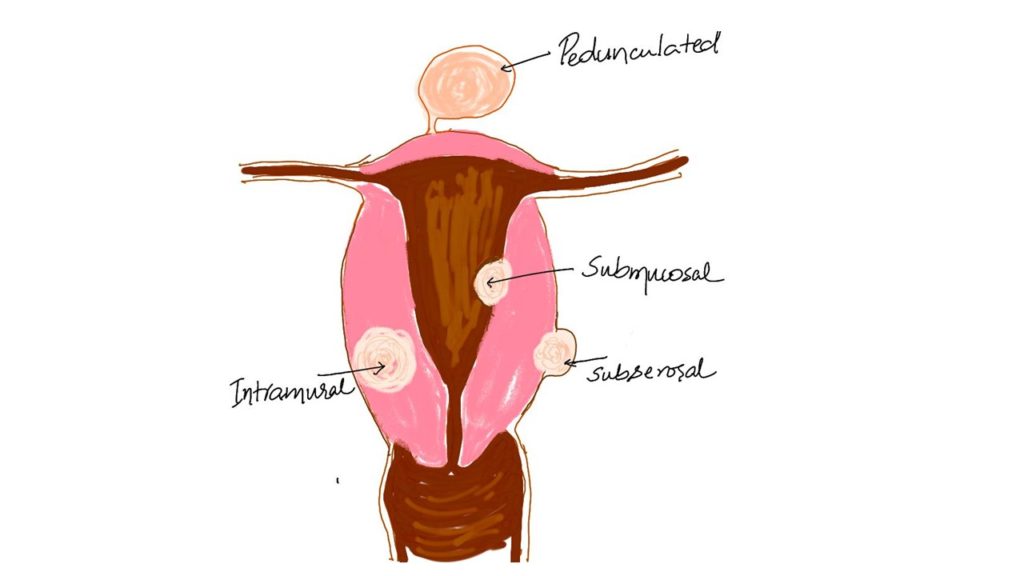
Based on the location of the tumor they are categorized as
1. Submucosal: present benath the endometrium. These are the ones which can manifest with menorrhagia.
2. Intramural: within the myometrium. These are usually asymptomatic if small and are often incidental finding.
3. Subserosal they are seen beneath the serosa. Can cause pressure symptoms due to compression on adjoining structures.
4. Pedunculated: Submucosal and subserosal tumors can be pedunculated with the presence of narrow pedicle.
Occasionally uterine tumors may detach and results in a rare type called PARASITIC leiomyoma.
Red Degeneration: This is due to hemorrhagic infaction of a leiomyoma. This is a complication usually occurs in pregnancy. The common cause is due to obstruction of venous drainage at the periphery of the lesion. This is also referred to as Carneous degeneration.
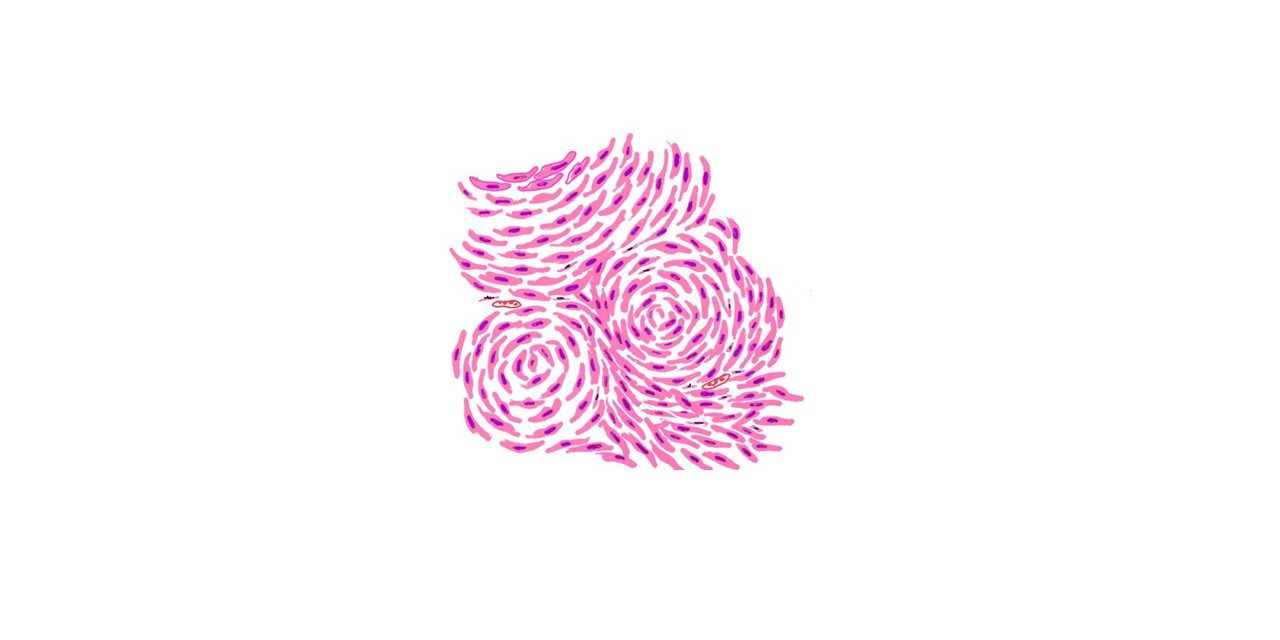
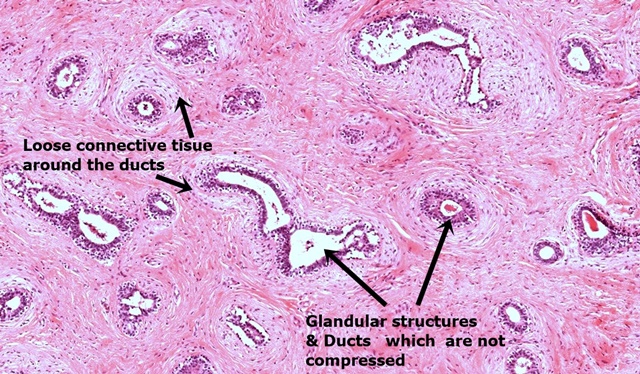
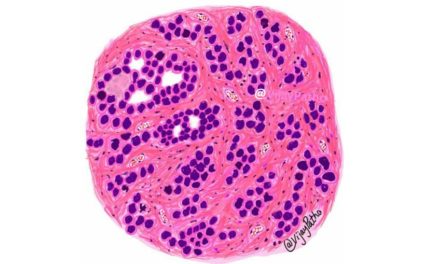
Microscopy: the pattern is that of interlacing fascicles or whorling of smooth muscle cells. The individual smooth muscle cells are uniform in size and shape and have characteristic oval to elongated with blunt ends ( CIGAR shaped). The cytoplasm s abundant and eosinophilic with elongated bipolar processes.
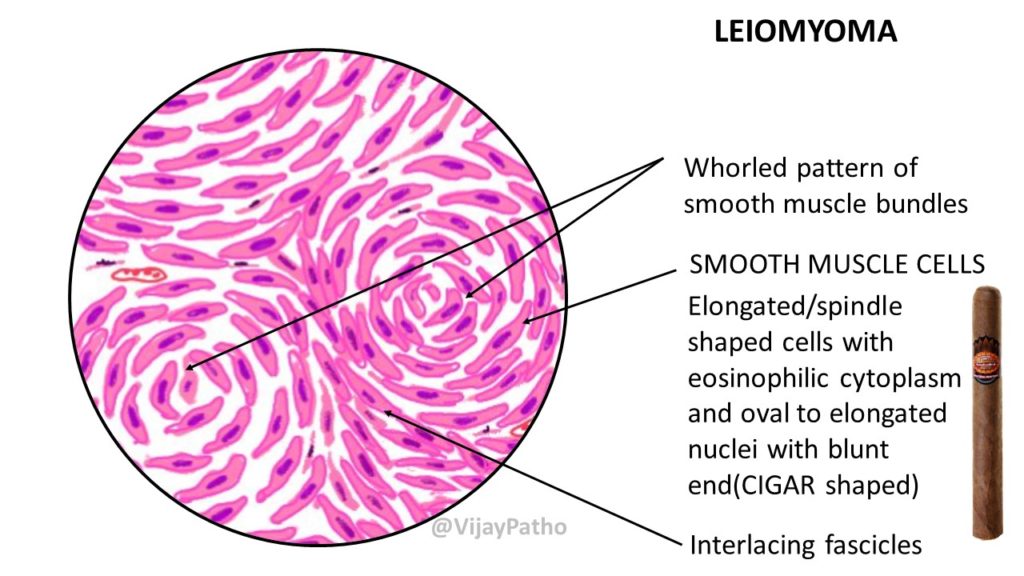
There are many microscopic variants which include cellular, Leiomyoma with bizzare nuclei, Mitotically active, hydropic, apopletic, lipomatous, epithelioid, myxoid, dissecting leiomyomas etc.





Recent Comments