This Video tutorial will help you in understanding the etiopathogenesis, morphology and complications of Hashimoto’s Thyroiditis
Salient Points:
Hashimoto’s thyroididtis
Most common cause of hypothyroidism in areas where iodine levels are sufficient.
Gradual thyroid failure due to autoimmune destruction of thyroid gland
Definition:It is Characterized by
1. Diffuse goitrous enlargement of the thyroid
2. Lymphocytic infiltration of the thyroid gland
3. Presence of thyroid autoantibodies.
Age incidence: 45 – 65yrs. Male: Female: 1:10 to 1:20
It can occur in children and is a major cause of nonendemic goiter in children.
1. Genetic predisposition.
2. Immune causes: Autoantibody production
3. Environmental factors: In a genetically susceptible individual environmental factors, such as infection, dietary factors (iodine) and stress due to hormones
Immune causes
Immune Regulatory Genes
[CTLA4, PTPN22]
cytotoxic T lymphocyte–associated antigen-4 (CTLA4)
protein tyrosine phosphatase-22
Thyroid specific genes
(thyroglobulin and thyroid-stimulating hormone [TSH] receptor )
GROSS
-Diffuse enlargement , may be Nodular
– Gland well demarcated Cut section; Pale, yellow tan, rubbery to firm/nodular
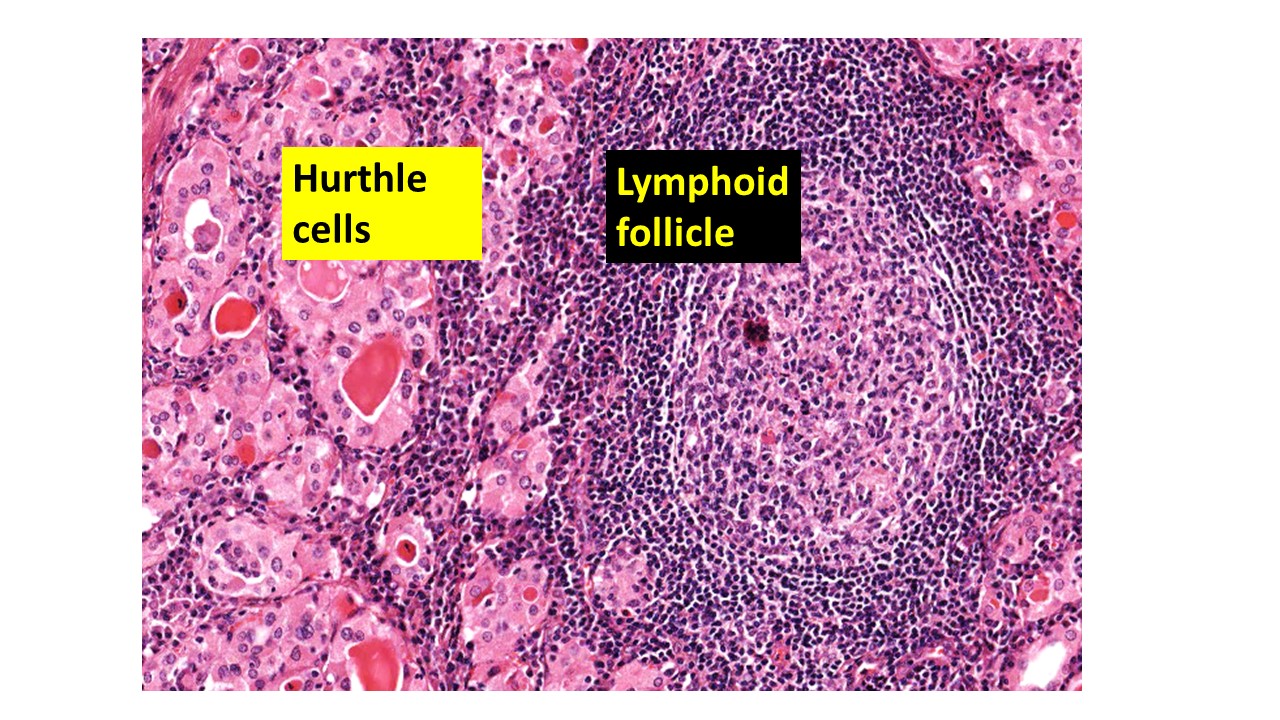
MICRO
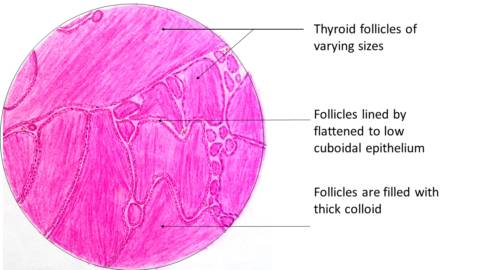
Atrophy of the follicles
Diffuse infiltration by mononuclear cells
Formation of lymphoid follicles
Hurthle cell metaplasia
Interstitial connective tissue may be increased
Clinical features : Middle aged women
Painless enlargement
Variable degree of
hypothyroidism
Laboratory findings: T3 & T4 decreased
TSH increased
Antithyroid antibodies
Diagnostic tests: FNAC
HPE of Biopsy
COMPLICATIONS
Hashitoxicosis
B-cell Non Hodgkin Lymphoma
Increased risk for other autoimmune diseases
Diabetes type 1, Adrenalitis, SLE, Myasthenia Gravis..
Increased risk(variable) thyroid epithelial neoplasms.. Papillary Carcinoma





Recent Comments